
The OIUF Fellowship at the Massachusetts Eye Research and Surgery Institution (MERSI) offers unique opportunities for education, training, and research for the care of patients with destructive ocular inflammatory diseases. OIUF has programs available for current medical students, recently graduated medical students, internationally trained ophthalmologists, and ophthalmologists with a Massachusetts state medical license. All fellows are obligated to perform the duties described in the MERSI Ocular Immunology Fellowship Guidelines. Upon successful completion of a fellowship, Fellows will receive a certificate from MERSI as well as a plaque to recognize this achievement.
OIUF Fellowship Program Opportunities
The OIUF Clinical Fellowship program is offered to those who have completed an Ophthalmology residency and have (or obtain) a license to practice medicine in the State of Massachusetts. This program is compliant with the Association of University Professors of Ophthalmology (AUPO FCC compliant). Each fellowship is a year-long position.
How to Apply:
How to Apply:
For any additional information with regard to OIUF’s Ocular Immunology Fellowship Program at MERSI, please contact: Scott Evans, (sevans@mersi.com).
The Ocular Immunology and Uveitis Foundation (OIUF) Fellowship Guidelines are presented here:
The primary goals of the OIUF Fellowship at MERSI are to develop diagnostic and therapeutic skills in caring for patients with destructive ocular diseases mediated by abnormal immunoregulatory or infectious processes, and to develop an information base in basic ocular immunology, with associated research skills, to facilitate appropriate total care of patients with ocular inflammation and any associated secondary comorbidities.
The specific goals and objectives enumerated below should serve as a starting framework:
Basic Objectives
Differential diagnosis, evaluation for formulation of diagnostic strategy, and total management of the following diseases:
The Fellow should reasonably be expected to have mastered these objectives within six months of his/her experience in the Fellowship; he/she should then develop further skills with some of the more difficult and subtle forms of immunologically mediated destructive ocular disease, and obtain experience in the indications for use of immunosuppressive agents. It is to be emphasized that the proper, safe use of cytotoxic drugs requires significant medical training and experience, and significant, frequent, longitudinal experience in the use of cytotoxic agents, recognition of complications induced by these agents, and management of such complications.
Our teaching emphasizes the case method approach in which each patient is to be examined initially by the Fellow and then formally presented to the attending staff member for discussion of diagnosis and treatment. Additional readings and pertinent references will often be suggested to supplement the attached basic list of reference material. Used properly, this experience will provide the opportunity for recognition and diagnosis of disease and will be the stimulus for in depth reading about each disease entity.
Additional complements and obligations to the educational program in the OIUF Fellowship include bi-weekly research meetings, participation in lectures and conferences, and the publication of several manuscripts. Lectures may be held by clinic faculty or visiting faculty. Each fellow is also responsible for presenting at least one lecture to their peers and faculty.
Dr. C. Stephen Foster is the President and Founder of the Ocular Immunology and Uveitis Foundation (OIUF). The OIUF executive board is made up of physicians and other contributing members with a dedicated interest in furthering the mission of this foundation.
III. Clinical Activities
Clinic is in operation Monday through Friday as well as on one Saturday per month. Additionally, on call fellows are responsible for the care of any patient seeking care any time the clinic is closed, with initial patient contact via the clinic’s answering service and telephone triage of the patient by the fellow. Examination of the patient may be necessary if it is decided that the matter is one deserving of urgent care.
The Fellow should attempt to make a diagnosis or at least place the case into as carefully-described a category as possible. Each new patient should be administered the Uveitis questionnaire, and a small general battery of laboratory tests should be ordered: CBC with differential, renal and liver function testing, sedimentation rate, microscopic urinalysis, urinalysis, and treponemal studies would be the usual minimum. Further studies are based on the results of the history and physical examination and on discoveries from the Review of Systems questionnaire.
Emergency or scheduled admissions for medical workup, for medical therapy, for diagnostic vitrectomy, or for emergency corneal, scleral or conjunctival surgery will be the responsibility of the Fellow on call. He/she is responsible for the admitting note, orders, daily rounds, assembling laboratory data, arranging post-discharge care details and completing the medical record. The assistant is responsible for completing the pathology form and dictating the operative note immediately after assisting in surgery.
The on-call Fellow is responsible for all emergency consults. These may be cases urgently referred from abroad, or from local practitioners, or they may be requests for consultation on inpatients at affiliated hospitals. Such consultations are to be presented immediately to the on-call attending.
There will typically be a Fellow designated as Lead Fellow whose responsibilities include organization of the on-call Fellow schedule, designation of clinic and research time for all Fellows, and, with the assistance of the attendings, development of the clinical lecture schedule and laboratory meetings, including journal club, case discussions, and other group meetings.
All Fellows should be aware that their time in the clinic is expected and that patient appointments and scheduling are in part determined by these expectations. A schedule for clinical duties and research time will be crafted by the designated Lead Fellow. Any requests for time away from clinic must be given in advance and approved to accommodate for this. Emergency situations for time away will always be considered but may not be guaranteed to be approved.
Our major goal is to provide a resource for individuals who are determined to become the best that they’re capable of becoming: from a personal, character point of view, as well as from a physician/clinician/caretaker point of view and from a restless, question-asking, scientist point of view.
This Program is not about excellent ocular immunology, or excellent ophthalmology; it isn’t even about excellent medicine. This program is about personal excellence. Excellence in attitude, behavior, and relationships. Our job is to cultivate the environment and resources to create the possibility and stimulation for each Fellow to grow to his or her maximum potential.
The resource that we have attempted and continue to attempt to provide for such individuals is comprised of an atmosphere that encourages generosity, thoughtfulness, kindness, consideration, respect; one that encourages independence, courage, with appropriate limits and circumspection, appropriate introspection and recognition of one’s knowledge and skills, and the feeling of complete comfort in recognizing and admitting to others what one does not know, asking for help, and graciously accepting help. We have tried to construct an environment that is rich in clinical material, so that physicians can appreciate the relevant human circumstances and ocular inflammatory diseases which need our attention, and can imagine possible ways for learning more about those important problems, and can develop exceptional expertise at recognizing (diagnosing) and treating those problems. The environment that we have attempted to create is one that includes a laboratory resource which is rich in opportunity and is stimulating from both a scientific and social perspective. The environment also includes teachers, “professors,” whose primary function is to stimulate, guide, critique and evaluate.
We hope that each Fellow will learn to identify a problem appropriate for study, map a strategy for solving that problem, and identify the resources necessary to pursue that strategy—whether the necessary resources are within or outside the OIUF Laboratory. Once the time has “apparently” arrived to begin an experiment, careful re-evaluation may disclose that, in fact, it is not time to begin. Planning, details, checking, rechecking, and then checking once again can save thousands of dollars and hundreds of wasted hours. Avoid the temptation to rush. Avoid the temptation to attempt to do too much in one experiment. Avoid the temptation to take short cuts. Even such seemingly safe expedients as using solutions or buffers that a colleague has been using, or relying on unverified or incomplete database material, have destroyed months of effort by some Fellows.
The level to which we succeed in our goal is mirrored by the behaviors of the individuals completing the Fellowship training program: behaviors both from a character/social perspective and from a clinician/scientist perspective. We have reason, so far, to believe that the program accomplishes its goal. Some Fellows take more with them from this environment than do others. All, however, have selflessly recognized the quid pro quo for the benefits they derive from the program: 100% dedicated effort to the Fellowship training program while in it, total commitment to the patients for whom they are responsible, and absolute honesty and scientific integrity.
Each Fellow may choose to work on a research project. There are few general services. Techniques such as tissue culture, histopathology, immunofluorescence and biochemical analyses can be taught to you, but, thereafter, you should do the work independently.
Research, presentation, and/or publication of interesting cases or series by fellows is strongly encouraged. We believe that a doctor is a better physician as a result of carefully analyzing a case, reviewing the literature, and reporting the case, than by not doing so. We also have the opportunity to present to the scientific community new and/or rare cases and the outcomes associated with our care.
Clinic records, kept in the electronic medical record files, may be reviewed upon approval of the project and, if necessary, upon obtaining IRB approval from the New England IRB. Most of you will be required to review patient charts for your clinical projects. There is an electronic medical record system which creates a cohort of patients according to specific ICD-10 codes, medication names, diagnoses, and more. For example, if you would like to review all charts for patients with keratoconjunctivitis, you can run a simple report within this system to identify all patients who have been seen at our clinic with this disease.
Fellows are strongly encouraged to present research findings at academic conferences. When an abstract is accepted either as a poster or oral presentation, a travel stipend will be provided if such travel is approved.
There is no such thing. Remember that. Think about that. Your time here is brief; don’t waste it. There will be many opportunities to waste it, many opportunities to be seduced by Boston, New England, etc. The array of saboteurs is endless. Read regularly. One hour a night, every night, without fail. Be systematic and you will consume an enormous amount of material in a year.
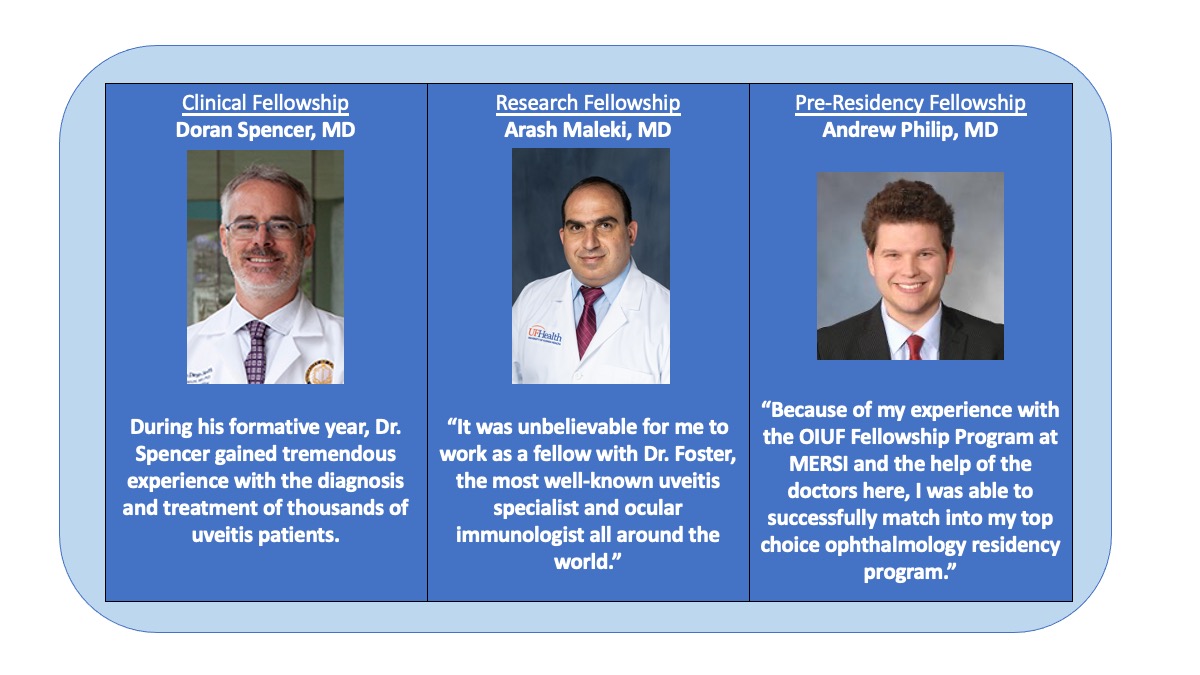
Testimonials
Pre- Residency Fellowship
Drew Philip
I came to the OIUF Fellowship Program after graduating medical school in order to bolster my application to ophthalmology residency programs. To say it was an incredible experience is an understatement. Working in the clinic at MERSI vastly improved my ophthalmology knowledge base, both in general and specifically in ocular inflammatory disease. The teachings of the attendings significantly improved my clinical skills far beyond what I had imagined was possible when I first started. I was also able to be involved in a significant amount of clinical research, both helping with ongoing projects and initiating projects of my own. This amounted to numerous peer-reviewed publications and presentations at both regional and national meetings. At the end of it all, I was able to match into an ophthalmology residency program that I was passionate about and was my top choice. With my newfound knowledge of ocular inflammatory disease, I am planning on specializing in this field upon completing my residency training.
Click here to listen to
Uveitis and Steroid-Sparing Therapy
Presented by C. Stephen Foster, MD, FACS, FACR
Audio-Digest Ophthalmology Volume 56, Issue 15
