 What is uveitis?
What is uveitis?
What is a slit lamp?
Anatomy of the eye
Pictures of the eye
Why does the doctor check my eye pressure?
What is a cataract?
How do blood cells fight disease?
Uveitis Glossary
EYE-word Puzzle
How to use eye drops
Fighting Back

Uveitis is inflammation inside the eye, in one or more of the three parts of the middle layer of the eye called the “uvea.” Uveitis is like having inflammation from a burn, but inside the eye.
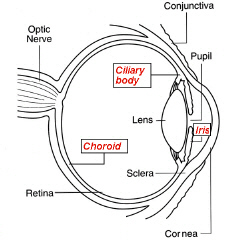
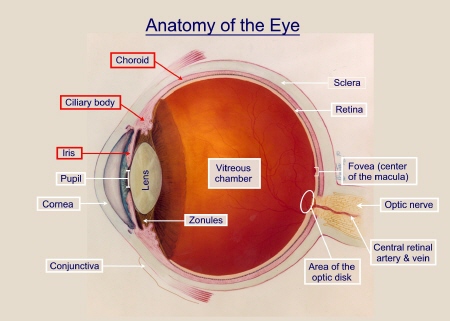
The uvea, or “uveal tract,” has three parts: the iris, ciliary body, and choroid.
![]() Uvea is the Latin word for grape. If you could see it, this part of the eye might remind you of a grape; it is brown and round, with a “stem” formed by the optic nerve.
Uvea is the Latin word for grape. If you could see it, this part of the eye might remind you of a grape; it is brown and round, with a “stem” formed by the optic nerve. ![]() Itis is the Latin suffix for inflammation. Put the two words together:
Itis is the Latin suffix for inflammation. Put the two words together:
![]() uve + itis = “uveitis”
uve + itis = “uveitis”
Uvea is the Latin word for grape. The term uveal tract has been given to the vascular middle layer of the eye because its structure is brown and spherical, and it resembles a grape, with the optic nerve forming the stalk.
The uveal tract is composed of iris, ciliary body, and choroid. Each of these components of the uvea has a unique histology, anatomy, and function. The uvea is the intermediate of the three coats of the eyeball, sandwiched between the sclera and the retina in its posterior (choroid) portion.
Anteriorly, the iris controls the amount of light that reaches the retina, whereas the ciliary body is primarily responsible for aqueous humor production. The ciliary muscle changes the curvature of the lens through the fibers of the zonular ligament. This makes the lens thicker so the eye can focus on nearby objects and thinner so the eye can focus on distant objects. The choroid is the sole blood supply to the avascular outer part of the retina. The highly vasculerized tissues of the choroid can be affected by systemic as well as local disease processes. In this diagram, the structures of the uvea are shown in red.
Click and Learn
In the “Uveitis Glossary” you can see pictures of the anatomy of the eye and look up words or terms that you want to know about.
Eye anatomy: How many parts of the eye can you name?

Inflammation is a characteristic reaction of tissues to injury or disease. It is marked by four signs: swelling, redness, heat, and pain.
Uveitis is inflammation inside the eye, like having inflammation from a burn, but inside the eye.

![]() The first doctor to describe uveitis, Imhotep, lived in Egypt around 2640 BC. He was a physician and architect who helped build pyramids.
The first doctor to describe uveitis, Imhotep, lived in Egypt around 2640 BC. He was a physician and architect who helped build pyramids.
![]() 5% to 10% of all cases of uveitis occur in children under the age of 16.
5% to 10% of all cases of uveitis occur in children under the age of 16.
![]() Uveitis can be treated.
Uveitis can be treated.
![]() Doctors need a special microscope, called a slit lamp, to examine the inside of the eye.
Doctors need a special microscope, called a slit lamp, to examine the inside of the eye.
Back to Top of Page | Next
How many parts of the eye can you name?
![]()
Jeff wants to know: What is a Slit Lamp and how does it work?
Your eye doctor uses a special kind of microscope, called a slit lamp microscope, to look inside your eyes. For short, it is called a “slit lamp”. The slit lamp has a beam of light that can be adjusted. By changing the width of the beam, the doctor can gather important details about your eyes.
![]() Have you ever looked through a microscope or a magnifying glass? If you have, you know that these magnifiers will make things look really BIG.
Have you ever looked through a microscope or a magnifying glass? If you have, you know that these magnifiers will make things look really BIG.
![]()
![]()
![]()
![]()
![]()
![]()

Bridget is resting her chin on the chin rest and her forehead on the white strap. This helps her hold her head still.
Dr. Foster is looking through the eye piece, through the lens of the slit lamp, into Bridget’s eye. Nothing touches Bridget’s eye.
Can you see the bright beam of light shining on Bridget’s eye, right in the center (the yellow spot)? Dr. Foster needs this light to be able to see inside her eye. Without the light, the eye would appear black or dark.
Dr. Foster can adjust the magnification of the slit lamp, and the angle of the light beam, and how bright the light is, by moving some of the dials and levers on the slit lamp.
 The eye is really, really beautiful when viewed under magnification.
The eye is really, really beautiful when viewed under magnification.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Interactive Drawing of the Eye
This is a great learning tool for kids and adults alike.
Move the magnifying glass around to explore (enlarge) parts of the diagram. Source: NIH
To learn more about uveitis, use the Uveitis Glossary.

Structures in the eye
Static drawing of the whole eye, showing the location of the cornea, pupil, iris, lens, retina, and optic nerve. Source: NIH
To look up these terms, use the Uveitis Glossary.

Structures in the front of the eye
Black and white diagram showing the cornea, pupil, iris and lens. Source: NIH
To look up these terms, use the Uveitis Glossary.

Structures in the back of the eye
Black and white diagram showing the location of the macula and fovea. Source: NIH
To look up these terms, use the Uveitis Glossary.
Tears
The function of tears is to bathe, lubricate, and nourish the surface of the eye. Tears also contains antibodies that help protect the eye from infection. Tears are produced by the lacrimal (tear) glands, located near the outer corner of the eye. The fluid flows over the eye and exits through two small openings in the eyelids (lacrimal ducts); these openings lead to the nasolacrimal duct, a channel that empties into the nose. The eye’s tears are composed of three layers: oil, water and mucus.

Animation of how the “aqueous” flows out of the eye
Did you know? In a healthy eye, the fluids in the front of the eye are exchanged about 10 times a day. If something happens to disrupt this amazing system, pressures inside the eye can rise dramatically. Fluids are produced in the ciliary body, and exit the eye through a delicate meshwork that surrounds the iris.
Back to TopDear Kerry,Kids that have uveitis do need to have their eye pressure checked at each visit. You are right. This is why. There is a part of your eye that is always making fluid; not tears, but fluid for the inside of your eye Isn’t that amazing? I think so.Doctors give this fluid a special name. It is called “aqueous.” Aqueous means water, and that is just what this special fluid inside your eye looks like. Aqueous helps your eye keep its shape and carries nourishment to the iris, cornea, and lens. Aqueous is crystal clear and easy to see through under normal conditions inside the eye. What part of the eye makes aqueous?
Back to Top Not to try to be silly, but the ciliary body (pronounced SILLY-air-ee) makes aqueous! The ciliary body sits just behind the iris, the colored part of your eye. Can you find the ciliary body in the drawing?Since aqueous is being made all of the time, you might wonder why your eye doesn’t get bigger and bigger!
Back to TopThat is because as new fluid is made, old fluid drains out of the eye. Aqueous fluid drains out of the eye through tiny openings. Follow the path of the red arrows in the drawing to your right to see the path of the fluid. The aqueous fluid inside a normally functioning eye gets exchanged about ten times a day.
The CORNEA is the clear dome through which the IRIS can be seen
(the iris is the colored part of the eye).
Aqueous fluid is made by the ciliary body and drains out of the eye through a system of tiny, tiny canals. Follow the red arrows so see its path.
If the tiny outflow drains get plugged up, pressure inside the eye will go up (get higher). If this were to happen, your eye doctor would give you a medicine to help get everything working well again.Sometimes, but not often, children who have uveitis develop problems with the pressure inside one or both of their eyes. To be sure that your eyes are making enough aqueous and that the aqueous drains are working well, you doctor will ask that your eye pressure be checked at every visit.Kids wonder if it hurts to get eye pressure checked. It should not hurt to get your eye pressure checked. A nurse will put eye drops in your eye. The eye drops will make your eye feel numb for a short while. Then, a tiny, special, tube-like medical instrument will touch your numb eye. You can’t feel it touch your eye, but you will be able to see what the nurse is doing. Your part is to ask any questions you have, then sit very still and keep your eye wide open so the nurse can do the test.Thank your, Kerry, for sending your question to the EYE-brary.
make your eye feel numb for a short while. Then, a tiny, special, tube-like medical instrument will touch your numb eye. You can’t feel it touch your eye, but you will be able to see what the nurse is doing. Your part is to ask any questions you have, then sit very still and keep your eye wide open so the nurse can do the test.Thank your, Kerry, for sending your question to the EYE-brary.
Dear Marcus,
A cataract, very simply, is any opacity (cloudiness) in the normally crystal clear lens of the Inside the eye, there is a lens which helps us to focus on what we see. The lens is made mostly of water and protein. The protein is arranged to let light pass through and focus on the retina. Sometimes some of the protein clumps together and starts to cloud a small area of the lens. This cloudiness of the lens is called a cataract. eye. I believe it gets its name from the Greek word meaning “waterfall”, since the look of it to some ancient reminded him of the hazy, opaque look of water as it cascaded over a fall.
Over time, the cataract may grow larger and cloud more of the lens, making it more difficult to see. In the early stages, stronger lighting may lessen the vision problems caused by cataracts. At a certain point, however, surgery may be needed to improve vision.
Sometimes, but not always, children with uveitis develop cataract. This can happen because of the uveitis itself or can be caused by some of the the medicines used to treat uveitis (prednisone). Children with uveitis who develop cataract can have surgery to remove the clouded lens if their eye is “quiet” (not having a “flare up”), and if their eye has not had any inflammation for at least 3 months before the surgery.
Thank your, Marcus, for sending your question to the EYE-brary.
 The cell is the fundamental unit of life. Your health depends on what happens within the many different types of cells that make up your body. The immune system is a network of cells (and organs) that has evolved to defend the body against attacks by “foreign” invaders, like germs, that can cause illness. Under normal conditions, your immune system protects your body from diseases and infections by killing these harmful “foreign” substances that enter the body.
The cell is the fundamental unit of life. Your health depends on what happens within the many different types of cells that make up your body. The immune system is a network of cells (and organs) that has evolved to defend the body against attacks by “foreign” invaders, like germs, that can cause illness. Under normal conditions, your immune system protects your body from diseases and infections by killing these harmful “foreign” substances that enter the body.
Small white blood cells, called lymphocytes, are the soldiers of the immune system. These white blood cells flow around your body, on the lookout for germs. When an intruder germ is discovered, the white cell surrounds it and swallows it. Chemicals called enzymes inside the cell eat (digest) the foreign substance and the harmless remains are pushed out. This process is call “phagocytosis ” by scientists. White cells not only fight germs in the blood; they can change shape and slide out of the blood vessel into the surrounding tissue in search of germs. White blood cells consume anything that should not be in the body — dirt in the lungs, and even, though slowly, a splinter.
Sometimes the immune system breaks down. If that happens, we get sick. So, for example, one of the cause of uveitis is a breakdown in the immune system called an auto-immune reaction. In autoimmune uveitis, the immune system gets mixed up and mistakes some parts of the eye as “foreign” and attacks this eye tissue just as it would a germs or other “foreign” substances. Your doctor can actually see the results of this attack by looking in your eye through a slit lamp. What the doctor sees through the slit lamp when someone has uveitis is “cells”; these are white blood cells.

To learn more about cells and how the immune system works, click on these links
![]()
![]() Understanding the Immune System (NIH)
Understanding the Immune System (NIH)
Come back here often to read more stories. And, ask a parent or teacher if you can send us your ideas for the EYE-brary. What would you like to read about?
![]() Click here to send us and E-Mail
Click here to send us and E-Mail
with your ideas for EYE-brary stories.
Links to Material We Recommend on Other Web Sites
![]() This symbol indicates that material is linked to another website. We have checked the websites we link to and think they are good. But, website content can change at any time and websites don’t have to tell anyone that they have changed. So, please advise your child (or student) that, when leaving the Uveitis Kids Page, they should be sure to check the privacy policy of each new site they visit.
This symbol indicates that material is linked to another website. We have checked the websites we link to and think they are good. But, website content can change at any time and websites don’t have to tell anyone that they have changed. So, please advise your child (or student) that, when leaving the Uveitis Kids Page, they should be sure to check the privacy policy of each new site they visit.
A Big Look at the Eye ![]()
 How Dogs See
How Dogs See ![]()
The Nocturnal Eye
Taking a Good Look at Glasses ![]()
What is 20/20 Vision? ![]()
What Visual Impairment is ![]()
Taking a Good Look at Glasses ![]()
How to Take Care of Your Glasses ![]()
Why do People Have Red Eyes in Some Flash Photography? ![]()
Band-Aids and Blackboards ![]() – kids tell their stories about how they deal with rare illness at school. A fun web site with interesting stories.
– kids tell their stories about how they deal with rare illness at school. A fun web site with interesting stories. ![]()
This page features pictures sent in by kids who visit this website. The pictures tell a story. Click a picture to make it bigger.
My uveitis
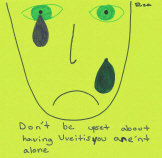
You aren’t alone
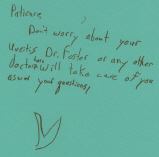
Somebody will be able to help you
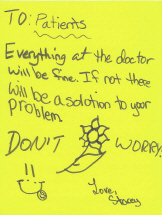
There will be a solution to your problem
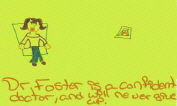
Dr. Foster is a confident doctor and will NEVER give up
Try not to be afraid
 We would like to put your drawing right here. Write to the webmaster, Liz Irvin. She will tell you how to send in your picture for the website.
We would like to put your drawing right here. Write to the webmaster, Liz Irvin. She will tell you how to send in your picture for the website.
 View projects done by other kids:
View projects done by other kids:

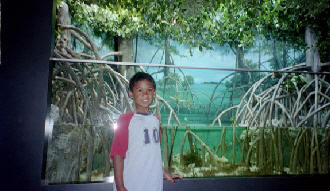
Hi. My name is Kian.
I am 7 years old. These are pictures from the trip that my mom and I took. We went to Boston to go to the Uveitis conference, AND we got to see a lot of cool things, AND eat a lot of peanut butter and jelly sandwiches. Yum! Yum!

Here’s a picture of the San Francisco airport. Our plane was going to take off from Gate 28. You can see that Gate here.

That’s me at the Logan airport in Boston. We were waiting for a van to pick us up and take us to our hotel!


The clock tower was my favorite building. You could see it no matter where you were in downtown Boston. I wish we could have gone in it.
OUR BOSTON ADVENTURES – THERE’S A LOT OF HISTORY HERE
 This is me and a guy dressed up as Benjamin Franklin. He really loves the United States.
This is me and a guy dressed up as Benjamin Franklin. He really loves the United States.
 This was a toy store in Quincy Market. The picture is of a big bionicle made all of legos. Quincy Market is a market full of tons of different kinds of food stores like Starbucks, seafood, pasta, smoothies and much, much more. This is Faneuil Hall, where some of the weapons from the revolution now are. This was the meeting place for the revolutionaries. It was funny to think that George Washington had stood right where we stood!
This was a toy store in Quincy Market. The picture is of a big bionicle made all of legos. Quincy Market is a market full of tons of different kinds of food stores like Starbucks, seafood, pasta, smoothies and much, much more. This is Faneuil Hall, where some of the weapons from the revolution now are. This was the meeting place for the revolutionaries. It was funny to think that George Washington had stood right where we stood!
 This is Faneuil Hall, where some of the weapons from the revolution now are. This was the meeting place for the revolutionaries. It was funny to think that George Washington had stood right where we stood!
This is Faneuil Hall, where some of the weapons from the revolution now are. This was the meeting place for the revolutionaries. It was funny to think that George Washington had stood right where we stood!

This ship is the USS Constitution. This boat has never lost a battle. They say it’s because there are cannons all around the boat. Other boats did not have cannons all around. It was the only boat during those times strong enough to withstand the weight of all the cannons. That’s how it won all the battles. It has special thick, hard wood to make it float and not leak.

These are two pictures of the park, Boston Commons. Can you guess which picture was taken at lunchtime?

These are two pictures of the park, Boston Commons. Can you guess which picture was taken at lunchtime?
 Here are pictures from the cemetery where a lot of people from the revolutionary era are buried.
Here are pictures from the cemetery where a lot of people from the revolutionary era are buried.

This is the old State House. Paul Revere originally covered the dome with copper (he was a blacksmith). Now it is covered in gold.
 Here’s me and my Uncle in front of Faneuil Hall. This is where you can see jugglers and other street performers. They were funny.
Here’s me and my Uncle in front of Faneuil Hall. This is where you can see jugglers and other street performers. They were funny.

Here are pictures from our harbor cruise. Can you see the United States flag waiving? Can you see the ship the USS Constitution? Can you see the cannons? Pretty cool!

 These are pictures from the Children’s Museum. I played in the two-story play structure and tried to hide from my Mom. There was water play where there were boats. We watched a play that some of the audience volunteered to be in. It was funny. It was the 3 Little Pigs.
These are pictures from the Children’s Museum. I played in the two-story play structure and tried to hide from my Mom. There was water play where there were boats. We watched a play that some of the audience volunteered to be in. It was funny. It was the 3 Little Pigs.

These are more pictures from the Children’s Museum. I played with the construction equipment there.
 This is me and my Mom at my favorite place to eat called Salty Dog. When my Dad went to college in Boston, he used to come here on Fridays and eat oysters. I don’t think he knew it, but they also have peanut butter and jelly sandwiches there. I loved them! We came here three times for them!
This is me and my Mom at my favorite place to eat called Salty Dog. When my Dad went to college in Boston, he used to come here on Fridays and eat oysters. I don’t think he knew it, but they also have peanut butter and jelly sandwiches there. I loved them! We came here three times for them!


This is me, Alexa, and her mom Renee at breakfast at the Holiday Inn before the Uveitis conference. It was the first time I met another kid with uveitis!
P.S. It was a really good breakfast!
 This is me waiting to see Dr. Foster.Can you see my blue registration card?
This is me waiting to see Dr. Foster.Can you see my blue registration card?

Dr. Topalkarg is the first doctor that saw me. That’s me jumping behind her as she’s working.

You can also see her examining my eyes.
 This is me and Dr. Foster. I almost love him because he did a lot for my eye.
This is me and Dr. Foster. I almost love him because he did a lot for my eye.
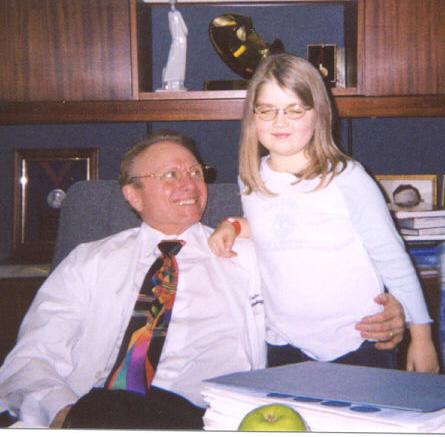
Alexa and her family traveled to Boston from Oregon to meet with Dr. Foster. Alexa was actually able to get Dr. Foster to sit down long enough to have this picture snapped. Alexa is great at getting people to smile (and, apparently, to sit down). Now, we all know that Dr. Foster wears gorgeous, colorful bright ties, and we look forward to “seeing” which one he will choose to wear next! BUT, we had forgotten to prepare Alexa about this one important fact . . . . . . . . . . . in his office, Dr. Foster’s ties shine especially brightly! Well, unprepared as she was, Alexa had to close her eyes for a split second. Oh! And, of course, that is exactly when her picture was snapped. Of course!
Alexa’s mom sent a note thanking ” . . . the Uveitis Support Group for helping us find Dr. Foster . . .” She and Alexa are members now, too, and send notes regularly through the “group’s” online connection, www.uosg.org. You can participate, too. Just click here and check us out.
Liz, who is a Boston member of the Support Group was really, really lucky to get to meet Alexa during her trip. and her mother and grandmother too; between appointments! Phew, what a long day they had.
This is Alexa’s grandmother Betty, new friend Liz, and Alexa’s mother, Renee. Didn’t Alexa do a great job taking this picture (and posing us for it)?


Liz and Alexa
What wonderful people. And, what an extraordinary journey they have undertaken. It was a privilege to meet all of them. And, we are still smiling here in Boston.
It’s 12 noon, 15 minutes left to 6th period math class. Mr. Butner, my eighth grade sequential one math teacher has been droning on for 83 minutes about quadratic equations. I look around the room and observe my fellow classmates, staring off into space and doodling in their notebooks. Then I realize it’s time for me to get out of class to do my 12:00 dose of Vexol. I guess that’s what’s called a bitter irony. 
Discovering my disease was a fluke. When I was 8, my mom took me to the eye doctor because one of my eyes looked like I was having an allergic reaction. After examining my eyes, the doctor actually found iritis in my other eye. The redness and itchiness had nothing to do with my disease, although ultimately I was diagnosed in both eyes. It was like someone had sent us a sign that something was wrong. If it was wasn’t for my mom and her “over-protectiveness” I would have begun to lose my vision. Thus started a long journey of doctors’ offices and prednisone eyedrops and dilating drops and monthly visits (and more) to the eye doctor.
I’ve seen so many eye doctors with so many opinions on what should be done about my iritis/uveitis in the past few years. It’s getting to the point where if I have to listen to my mom tell one more doctor my medical history, I’m going to become physically sick. Up until recently, I never felt that my disease was really impacting my life. So I had to do nine eye drops a day. I guess I got used to it. My mom and I would be driving home from an appointment after more cells were discovered and she would ask me, “Emily, how come you aren’t affected by this?” I would say that all it meant was another drop every day. It didn’t affect my daily life. But now I am fourteen, and my disease has definitely had an impact on my life. Last year when my eyes were being examined at a monthly appointment, my eye pressure had suddenly increased. I was given glaucoma drops, and everything has changed.
Now I’m on a drug to deal with this new problem because everything has changed. It’s called methotrexate. Methotrexate. It’s such a scary name for a drug that every ophthalmologist I’ve spoken to describes as a miracle drug. Why can’t they name it something else? Like, oh maybe, “Trixie?” Then on Sundays at 10:00 a.m. after breakfast I could say to my mom, “I’m taking my Trixie now!” Or at least something a little more kid-friendly. After all, there are a lot of kids, including me, who are depending on this drug to keep their eyes “quiet.”
To be perfectly honest, I’m not exactly sure how I feel about my disease. Some days I’m scared; some days I feel like going a little bit crazy and screaming and punching a pillow; some days I feel adrift and not totally connected to my situation. But on some rare days I feel strong and determined to beat this disease. I know I’ll do whatever it takes.

Bridget and Meredith Quirk carried the Olympic Torch on behalf of uveitis patients everywhere on December 27th, 2001 in Braintree, MA.
This wonderful event gave birth to the Bridget & Meredith Quirk Fundat the Massachusetts Eye and Ear InfirmaryThe fund fights pediatric blindness by targeting research into the causes and treatment of childhood uveitis. The Fund was established by Dan and Mary Jo Quirk in honor of their daughters, Bridget and Meredith, to raise money to purchase special laboratory equipment used to research inflammatory diseases of the eye such as uveitis.
The Fund was established by Dan and Mary Jo Quirk in honor of their daughters, Bridget and Meredith, to raise money to purchase special laboratory equipment used to research inflammatory diseases of the eye such as uveitis.
Uveitis is an illness that blinds thousands of children and adults every year in this country. The Fund supports the groundbreaking research that is carried out by C. Stephen Foster, M.D., Director of the Ocular Immunology Service and Laboratories at Massachusetts Eye and Ear Infirmary in Boston. Dr. Foster is a Professor of Ophthalmology at Harvard Medical School and the author of over 600 publications.
 The first goal of the Quirk family was to purchase a Heidelberg confocal laser scanning slit lamp biomicroscope. Through the help of generous donors that included local businesses, family, and friends, over $127,500 was raised for the fund, accomplishing the goal of purchasing the laser scanning slit lamp biomicroscope.
The first goal of the Quirk family was to purchase a Heidelberg confocal laser scanning slit lamp biomicroscope. Through the help of generous donors that included local businesses, family, and friends, over $127,500 was raised for the fund, accomplishing the goal of purchasing the laser scanning slit lamp biomicroscope.
We, Dr. Foster, the Uveitis/OID Support Group, and Massachusetts Eye and Ear Infirmary, are all deeply touched and grateful for the efforts of Mr. and Mrs. Quirk and Bridget and Meredith in raising this money to fight uveitis and ocular inflammatory diseases. Mr. and Mrs. Quirk did this not only for their daughter, Bridget, but for all children and adults who suffer with an ocular inflammatory disease.
How to Submit Material to the Kids Page
I was diagnosed with uveitis related to juvenile rheumatoid arthritis at age 11. My school detected vision loss on a routine exam. When I went to the ophthalmologist, for what we thought was glasses, the uveitis was diagnosed. Unfortunately, I was then inappropriately treated for ten years with steriods, which left me with a lot of structural damage in both eyes. My left eye is legally blind as a result. Thanks to Dr. Foster’s state of the art care and the starting of immunomodulators, my vision in my right eye was saved and I have been in remission for nine years.
I thought I would focus this story on those issues that change ones life, when you have a chronic illness, such as uveitis:
Frequent eye appointments/eye drops – I do not recall being negatively affected by either of these nor harboring any resentment. They became part of my routine and still are. I put my own eye drops in and managed my medications from the time I was diagnosed. When I became 19 or 20, it became extremely important for me to attend my eye doctor appointments alone, which my mother, although hesitant initially, did let me do.
Body Image Changes – In the seventh and eighth grade, my left eye became opaque secondary to my cataract and also the eye started to float outward. My male peers in school would tease and would ask each other within my hearing distance, who is she staring at, me or you? It was extremely embarrassing for me.
As a child, I was petite and because of the chronic steriod use, I gained a lot of weight. It started at that sensitive age of 12 -13 and I was very self-conscious of this weight gain. The same issue arose when I was in college. My steriods were increased over the summer break, and when I returned to school I was 5-10 pounds heavier. I heard my peers talking about how much weight I gained over summer break. I didn’t know how to deal with this, whether or not to let others know it was medication related. I found this to be very difficult to cope with.
My pupils were always uneven and when I was young, I was again very self-conscious of this defect. I worried that others would notice it and think I was odd.
Emotional Effect – I can’t remember emotions of my own when I was younger. I feel that it was because I didn’t understand what was happening. My emotions were always affected by my mother’s emotions. When I was first diagnosed, I only cried after I saw that my mother was crying. If my mother didn’t react, then I didn’t react.
I do remember being fearful in regards to my symptoms. I never had symptoms, initially. I saw floaters in my right eye several years after being diagnosed. I knew they were not right, but for whatever reason I was scared to tell my parents about them. I would initially be in denial, hoping they would go away. I don’t know why I was fearful and eventually I would tell.
As I grew older, I realized I was being led down the wrong path for treatment and became angry and started advocating for myself. I asked for a referral to another doctor, which eventually led me to Dr. Foster. When he first told me that I would be blind in a few years, if I didn’t move on with treatment and try immunomodulators, I was in shock as no one ever told me that before. I always heard, “it will burn out”. When Dr. Foster said, I needed immunomodulators, and I shook my head, no, out of fear. I was fearful of immunomodulators, thinking of them in terms of chemotherapy for treating cancer. I did a lot of reading and realized that they are safer than using steriods chronically. Unfortunately, I made my decision too late and suffered more structural damage to the eye. It took a while for me to internalize that this is a vision-robbing disease and prompt treatment is needed as, again, for ten years, I was told, “it would burn out”.
The last comment on emotional effect is a feeling of frustration by mother’s eternal optimism. I would try to vent to my Mom, regarding something going on with my eye, in hopes of sympathy. Unfortunately, my Mom would and still does say, “oh hunny, don’t worry about it, you’ll never go blind or you’ll be fine”. It’s now a standing joke and I’ve replaced the frustration with humor. However, I would still find emotional support, instead of optimism, more helpful to ease the pains of uveitis.
Loss of Vision and lack of Depth Perception – I was right eye dependent by the time I was diagnosed and never even noticed the vision loss in my left eye. I don’t remember what it was ever like to be binocular and have depth perception, so I’ve never miss it. I am grateful for what vision I do have and I don’t feel resentful that I couldn’t do certain things because of my vision.
In retrospect, as an adult with uveitis since my childhood, I don’t consider myself to be different from others because of having uveitis. I don’t think of my chronic illness of uveitis everyday nor weekly. Being in remission, helps to let go of the “what ifs”. I sometimes worry about loosing the vision in my only good eye from trauma or glaucoma, but I don’t dwell on it. My uveitis is a part of my life now. I often think that having grown up with it, I may even feel a void without it.
In thinking about what would have made my experience better, I would have to say, help in those aforementioned areas that I found difficult to cope with and to have had my feelings validated by my parents when I wanted to vent.
Child readers are invited to submit a drawing or other original work to The Gallery. Ask a parent or teacher, first, if it is OK to write to us about your project. If it is, write to the Kids Page Webmaster and tell us what you would like to submit. We will write back and tell you how to send your material.
It is O.K. to ask questions when you go to the doctor.
We encourage kids to ask questions about their eyes and health when they go to see their eye doctor. Sometimes it is helpful to write down questions ahead of time on a piece of paper and take that with you to your appointment. Tell your parents and your doctor what your questions are at each visit.
Scroll down the page, or click and choose:
If you would like to send a question for this page, click here
![]() What does “uveitis” stand for? What is uveitis? Inflammation inside the eye.
What does “uveitis” stand for? What is uveitis? Inflammation inside the eye.
![]() Is uveitis a bad eye disease for kids? If by “bad” you mean is uveitis a serious health problem, the answer is yes.
Is uveitis a bad eye disease for kids? If by “bad” you mean is uveitis a serious health problem, the answer is yes.
![]() Can uveitis be treated? Yes. We know a lot about how to help kids that have uveitis.
Can uveitis be treated? Yes. We know a lot about how to help kids that have uveitis.
![]() What causes uveitis? About 50 different things can cause uveitis.
What causes uveitis? About 50 different things can cause uveitis.
![]() What do I tell my 6th grade friends when they ask me what uveitis is? That it is inflammation inside the eye, like having inflammation from a burn, but inside the eye.
What do I tell my 6th grade friends when they ask me what uveitis is? That it is inflammation inside the eye, like having inflammation from a burn, but inside the eye.
![]() Is uveitis contagious? Can other kids “catch” uveitis from me? No.
Is uveitis contagious? Can other kids “catch” uveitis from me? No.
![]() How can I help my sister with uveitis? Let her talk to you about it. You don’t need to “do” or “say” anything. Just listen.
How can I help my sister with uveitis? Let her talk to you about it. You don’t need to “do” or “say” anything. Just listen.
![]() What are some of the various reasons for getting uveitis? If you have uveitis, are you considered an ill or sick person with a disease? Yes, uveitis is an illness. Infection, trauma, and autoimmune illness are the most frequent reasons that uveitis develops in children.
What are some of the various reasons for getting uveitis? If you have uveitis, are you considered an ill or sick person with a disease? Yes, uveitis is an illness. Infection, trauma, and autoimmune illness are the most frequent reasons that uveitis develops in children.
![]() Why can’t you see uveitis; is it only a eye disease, or can you develop it some other way? Doctors can “see” your uveitis with a special microscope called a slit lamp.
Why can’t you see uveitis; is it only a eye disease, or can you develop it some other way? Doctors can “see” your uveitis with a special microscope called a slit lamp.
![]() Are you scared that other kids might come to be blind from uveitis? No, not scared. But, concerned, which is why I do what I do.
Are you scared that other kids might come to be blind from uveitis? No, not scared. But, concerned, which is why I do what I do.
![]() Does everyone with uveitis have JRA? No.
Does everyone with uveitis have JRA? No.
![]() Does someone with uveitis have to have eye surgery? Sometimes, but not usually.
Does someone with uveitis have to have eye surgery? Sometimes, but not usually.
![]() Do you get scared when kids go into surgery that they will die? Not at all!
Do you get scared when kids go into surgery that they will die? Not at all!
![]() About how old will I be when my uveitis goes away? I don’t know.
About how old will I be when my uveitis goes away? I don’t know.
![]() On average, how long will I have uveitis; will it be until I am really old? We do not know; it is completely individual for each patient. But, it almost certainly will not last until you are really old.
On average, how long will I have uveitis; will it be until I am really old? We do not know; it is completely individual for each patient. But, it almost certainly will not last until you are really old.
![]() Will my uveitis change when I become a teenager (go through puberty)? Usually not.
Will my uveitis change when I become a teenager (go through puberty)? Usually not.
![]() Do some cases of uveitis last through adulthood? Usually not, but some do.
Do some cases of uveitis last through adulthood? Usually not, but some do.
![]() What is the longest period of time anyone has had uveitis? I don’t know.
What is the longest period of time anyone has had uveitis? I don’t know.
![]() Is uveitis a genetic disease? Usually not.
Is uveitis a genetic disease? Usually not.
![]() Was I born with uveitis? No.
Was I born with uveitis? No.
![]() Since I have uveitis, will my children have uveitis? Almost certainly not.
Since I have uveitis, will my children have uveitis? Almost certainly not.
![]() Will research find a cure for uveitis? Yes, we think so.
Will research find a cure for uveitis? Yes, we think so.
![]() Is methotrexate the most common treatment for uveitis?
Is methotrexate the most common treatment for uveitis?
No, steroids are.
![]() Will methotrexate keep uveitis from going into my other eye?
Will methotrexate keep uveitis from going into my other eye?
Yes
![]() How does the methotrexate help me? Why do I have to have blood tests?
How does the methotrexate help me? Why do I have to have blood tests?
Methotrexate kills the cells of inflammation, the ones inside the eye that do damage to the eye if they are allowed to stay. Blood testing is necessary so that your methotrexate dose can be increased or decreased if necessary to accomplish this goal.![]() When can I stop having blood test taken?When you are no longer taking medicine
When can I stop having blood test taken?When you are no longer taking medicine
![]() Sometimes I get tired. Is that a side affection of my medication?
Sometimes I get tired. Is that a side affection of my medication?
Probably.
![]() Once my uveitis is under control, when can I expect to taper off medicine?
Once my uveitis is under control, when can I expect to taper off medicine?
After two years with no uveitis.
![]() How long do I need to get check ups?
How long do I need to get check ups?
Until you no longer have uveitis and are not on any medicine.
![]() I often get sick just thinking about a medicine that’s trying to treat my uveitis. What can I do when I get that feeling?
I often get sick just thinking about a medicine that’s trying to treat my uveitis. What can I do when I get that feeling?
Talk to your mother and father about this. Since you know that this is “mental” (how you are thinking about your situation), see if you can find a way to overcome your fear, imagining, for example, the medicine killing the uveitis.
![]() Will my contact lens ever stick in my eye?
Will my contact lens ever stick in my eye?
Probably not.
The Uveitis Support Group maintains a free,
 safe, moderated spot on the web where kids who visit this web site can interact with each other online. This online kids club is a safe way for kids to write to each other without giving out E-Mail addresses.
safe, moderated spot on the web where kids who visit this web site can interact with each other online. This online kids club is a safe way for kids to write to each other without giving out E-Mail addresses.
A password is required to take advantage of the club’s safety features.
Request a Password by using this link to send an e-mail to the webmaster. Please ask your parents first if it is OK to write to us. We will write back and help you get registered.
The Kids Club is facilitated by our teen moderator, Olivia. Olivia lives in the state of Georgia in the United States. Our adult moderators are Liz Irvin, PhD, a member of the Uveitis/OID Support Group, and C. Stephen Foster, M.D. Come on. Join us. It’s lots of fun.
Click here to listen to
Uveitis and Steroid-Sparing Therapy
Presented by C. Stephen Foster, MD, FACS, FACR
Audio-Digest Ophthalmology Volume 56, Issue 15
