- TEARS
- TONOMETRY
- TONOMETER
- TRABECULAR MESHWORK
- TRABECULITIS
- TREATMENT ALGORITHM
- 20/20 VISION
- TYNDALL EFFECT (TYNEDLL PHENOMENA)
- VASCULITIS
- VISUAL ACUITY
- VISUAL FIELD
- VITRECTOMY
- VITREOUS
- VITRITIS
- VOGT-KOYANAGI-HARADA SYNDROME (VKH)
 The function of tears is to bathe, lubricate, and nourish the surface of the eye. Tears also contains antibodies that help protect the eye from infection. Tears are produced by the lacrimal (tear) glands, located near the outer corner of the eye. The fluid flows over the eye and exits through two small openings in the eyelids (lacrimal ducts); these openings lead to the nasolacrimal duct, a channel that empties into the nose.
The function of tears is to bathe, lubricate, and nourish the surface of the eye. Tears also contains antibodies that help protect the eye from infection. Tears are produced by the lacrimal (tear) glands, located near the outer corner of the eye. The fluid flows over the eye and exits through two small openings in the eyelids (lacrimal ducts); these openings lead to the nasolacrimal duct, a channel that empties into the nose.
The eye’s tears are composed of three layers: oil, water and mucus.
- The outermost, or lipid, layer provides an oil-based surface that retards evaporation of tears. This layer is produced by the meibomian glands which line the edge of the eyelids. If this layer did not exist, tears would evaporate 10 to 20 times faster than they do.
- The middle, or aqueous, layer includes salt and protein in a base that is 98% water. This watery portion of the tear film is produced by the lacrimal gland.
- The inner mucin layer coats the surface of the eye, allowing the other layers to form a film. Without this layer the tears would “bead up,” much like rain on a waxed car. The mucus layer comes from microscopic goblet cells in the conjunctiva.
When tears lack the important components described above, or when too few tears are produced, the tear film can break down. This breakdown produces dry spots on the cornea, causing the symptoms associated with dry eye – a feeling of itchiness, grittiness, a burning sensation, and general discomfort.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
TONOMETER, APPLANATION TONOMETER
 An instrument used to measure intraocular pressure. The applanation tonometer is considered the “gold standard” for measuring intraocular pressure.The patientçs eye is first treated with numbing drops and a stain called fluorescein. The tonometer is then placed gently on the cornea, and a very small amount of pressure is applied to the cornea.
An instrument used to measure intraocular pressure. The applanation tonometer is considered the “gold standard” for measuring intraocular pressure.The patientçs eye is first treated with numbing drops and a stain called fluorescein. The tonometer is then placed gently on the cornea, and a very small amount of pressure is applied to the cornea.
See, also, GLAUCOMA, GLAUCOMA AND UVEITIS
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The standard to determine the pressure inside the eye (intraocular pressure). The use of a device to measure the pressure in the eye.
See, also, GLAUCOMA, GLAUCOMA AND UVEITIS
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Inflammation of the trabecular meshwork.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
20/20 vision is a term used to express normal visual acuity (the clarity or sharpness of vision) measured at a distance of 20 feet. Someone with 20/20 vision can see clearly at 20 feet what should normally be seen at that distance. If a person has 20/100 vision, it means that they must be as close as 20 feet to see what a person with normal vision can see at 100 feet.
20/20 does not necessarily mean perfect vision. 20/20 vision only indicates the sharpness or clarity of vision at a distance. There are other important vision skills, including peripheral awareness or side vision, eye coordination, depth perception, focusing ability and color vision that contribute to your overall visual ability. Some people can see well at a distance, but are unable to bring nearer objects into focus. This condition can be caused by hyperopia (farsightedness) or presbyopia (loss of focusing ability). Others can see items that are close, but cannot see those far away. This condition may be caused by myopia (nearsightedness).
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
TRABECULAR MESHWORK (truh-BEC-yoo-lur)
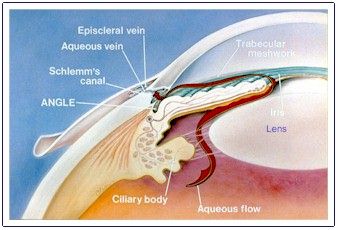
The trabecular meshwork is the spongy, mesh-like tissue surrounding the iris that allows the aqueous fluid (humor) to flow to Schlemm’s canal then out of the eye through ocular veins.
See, also, GLAUCOMA, GLAUCOMA AND UVEITIS
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
TREATMENT ALGORITHM (ALGORITHM)
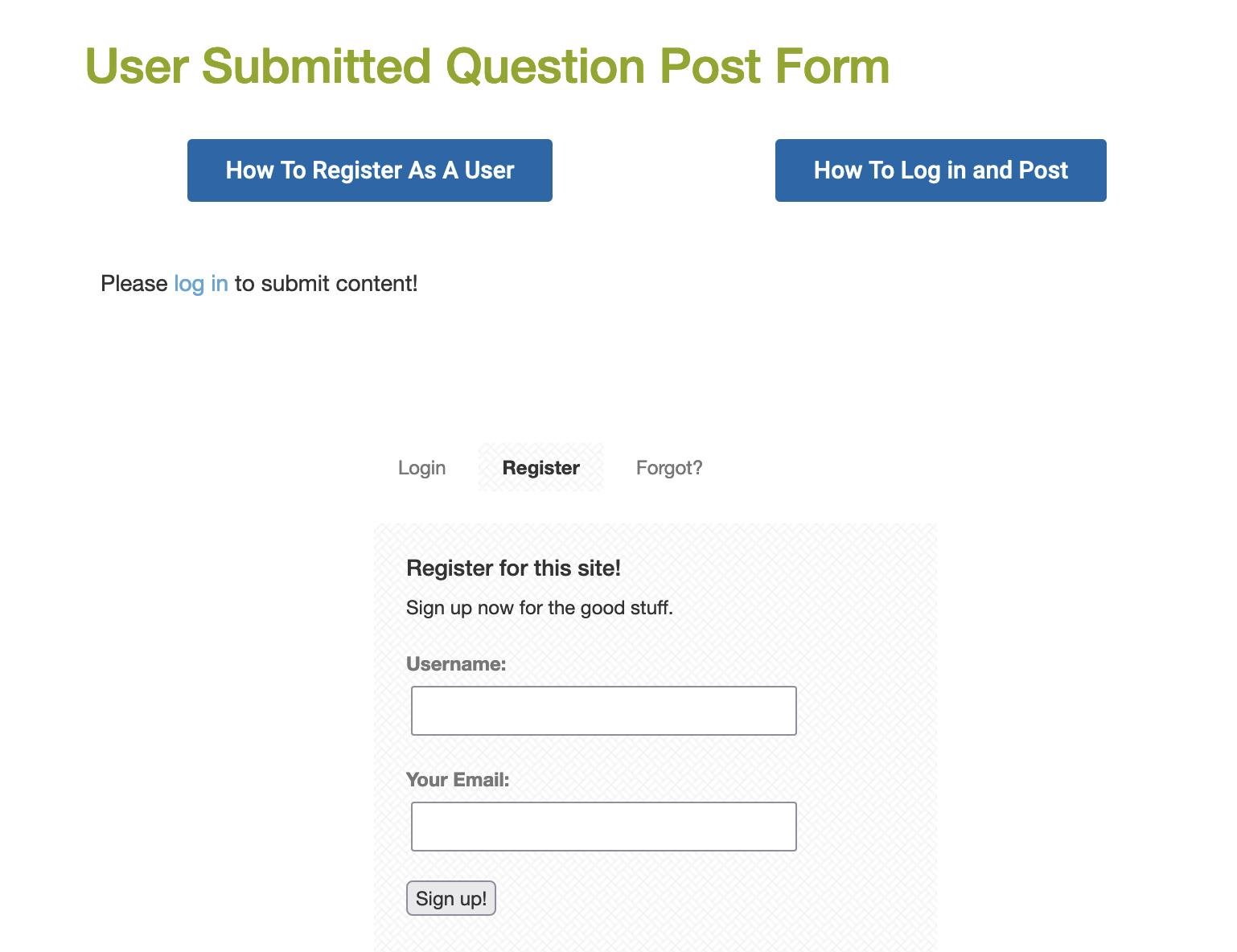
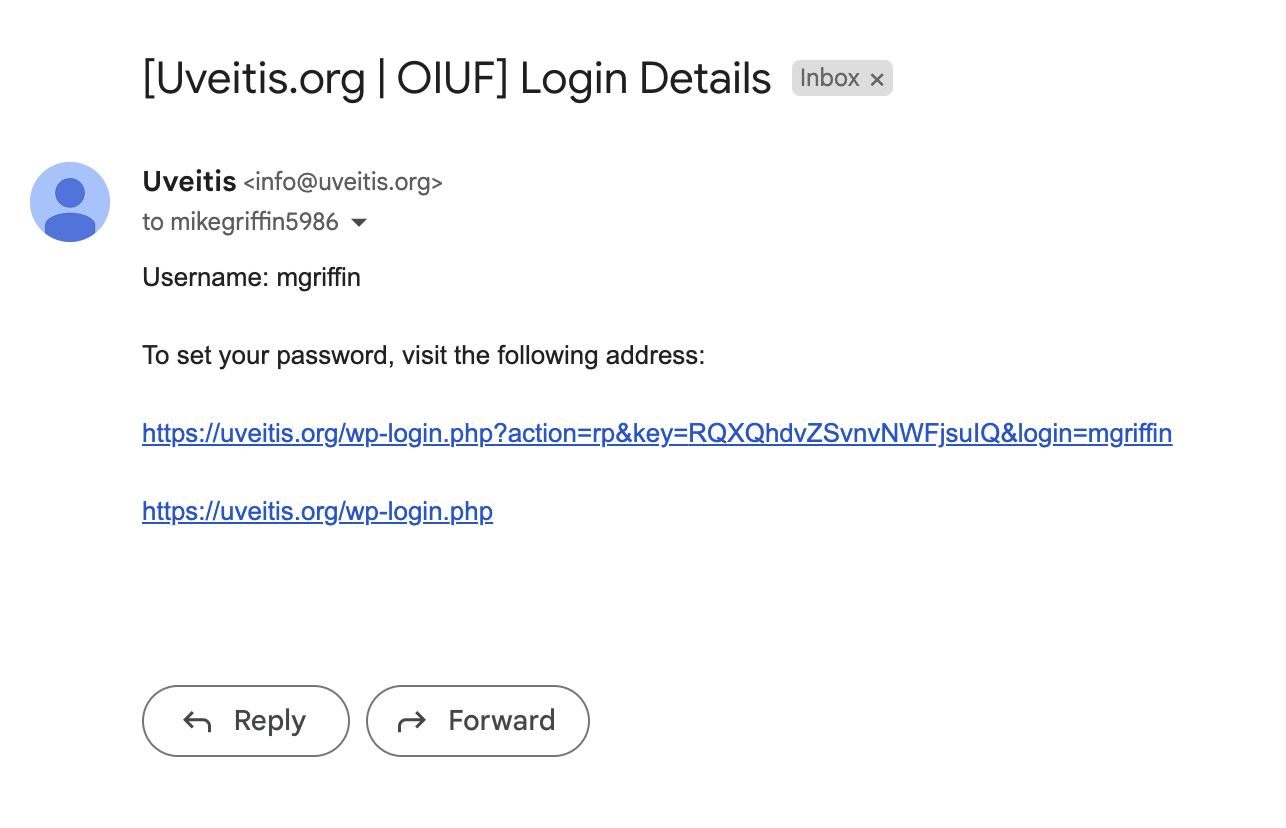
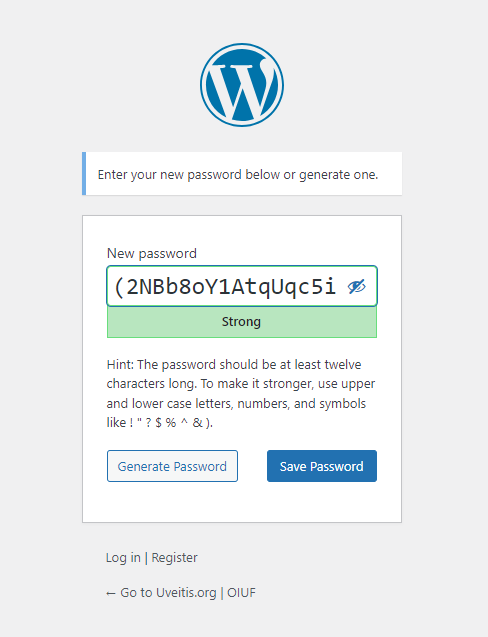
A description of the steps recommended in the care of a particular disease. A “step-ladder” approach to intervention. Treatment guidelines are meant as general guidelines for physicians. A great deal of judgment and experience is required in applying such guidelines to the care of any particular individual patient. Treatment algorithms for ocular inflammatory disease have been developed by the Massachusetts Eye Research and Surgery Institution , in conjunction with the Ocular Immunology and Uveitis Foundation, in Boston. Click here to review these algorithms.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Tyndall phenomena: the visibility of floating particles in gases or liquids when illuminated by a ray of sunlight and viewed at right angles to the illuminating ray. As an illustration, you have probably seen dust particles floating in the air when the sun is filtered through slatted blinds, scattering light into a room you are cleaning.
Example: the blue iris
Scattering of light (Tyndall effect and, closely related, Rayleigh scattering) can thus be observed quite frequently. The iris of the human eye does not contain any blue pigment or dye. The turbid front layer, if it contains no or only little melanin, appears blue in front of the dark back layer due to the preferred scattering of light with short wavelengths. Blue eyes are probably the best known example of Tyndall scattering.
Similarly, the slit lamp makes use of the Tyndell effect to illuminate particles that may be floating in the fluids inside your eye. Called “cells,” these particles are the byproducts of inflammation (white blood cells) and can be observed using the slit lamp as a light source. The number of cells are counted and form a system for rating the amount of inflammation.
CLICK AND READ:
Look the term “cells” in this Glossary (click on “C” in the index below)
Read more: What is a slit lamp?
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
UVEA, UVEAL TRACT (YOO-vee-uh)
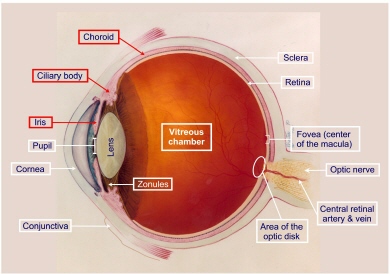
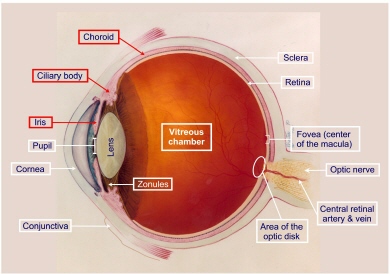 The uvea (from the Latin, uva or grape) is composed of iris, ciliary body, and choroid. Each of these components of the uvea has a unique histology, anatomy, and function. The uvea is the intermediate of the three coats of the eyeball, sandwiched between the sclera and the retina in its posterior (choroid) portion.
The uvea (from the Latin, uva or grape) is composed of iris, ciliary body, and choroid. Each of these components of the uvea has a unique histology, anatomy, and function. The uvea is the intermediate of the three coats of the eyeball, sandwiched between the sclera and the retina in its posterior (choroid) portion.
Anteriorly, the iris controls the amount of light that reaches the retina, whereas the ciliary body is primarily responsible for aqueous humor production. The ciliary muscle changes the curvature of the lens through the fibers of the zonular ligament. This makes the lens thicker so the eye can focus on nearby objects and thinner so the eye can focus on distant objects. The choroid is the sole blood supply to the avascular outer part of the retina. The highly vascularized tissues of the choroid can be affected by systemic as well as local disease processes. In this diagram, the structures of the uvea are shown in red.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
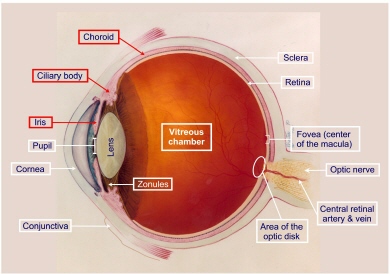 Uveitis is inflammation inside the eye, specifically affecting one or more of the three parts of the eye that make up the uvea: the iris (the colored part of the eye), the ciliary body (behind the iris, responsible for manufacturing the fluid inside the eye) and the choroid (the vascular lining tissue underneath the retina). The structures of the uvea, marked here in red, are collectively known as the uveal tract. Uveitis is a serious ocular condition. It is the third leading cause of blindness worldwide, accounting in the United States for 10-15% of all blindness. Untreated or under-treated uveitis, or repeated episodes of inflammation within the eye, can lead to scarring and blinding consequences. Uveitis is a treatable condition. Patients are urged to seek consultation with a uveitis specialist, a physician with advanced training in inflammatory eye disease.
Uveitis is inflammation inside the eye, specifically affecting one or more of the three parts of the eye that make up the uvea: the iris (the colored part of the eye), the ciliary body (behind the iris, responsible for manufacturing the fluid inside the eye) and the choroid (the vascular lining tissue underneath the retina). The structures of the uvea, marked here in red, are collectively known as the uveal tract. Uveitis is a serious ocular condition. It is the third leading cause of blindness worldwide, accounting in the United States for 10-15% of all blindness. Untreated or under-treated uveitis, or repeated episodes of inflammation within the eye, can lead to scarring and blinding consequences. Uveitis is a treatable condition. Patients are urged to seek consultation with a uveitis specialist, a physician with advanced training in inflammatory eye disease.
Inflammation of the uvea may occur as a consequence of diverse stimuli. These can be broadly classified according to the following mechanisms: traumatic, immunologic, infectious, and so-called masquerade. Uveitis may affect individuals of any age from infancy on. It also affects people from all parts of the world, and it is highly significant cause of blindness, accounting for 10-15% of all blindness in the United States. The average age (mean age) at presentation is approximately 40 years. Uveitis can affect people at virtually any age. Many patients in the pediatric age group, younger than 16 years, suffer devastating complications of uveitis. The peak age at onset of uveitis, in the third and fourth decades, magnifies the socioeconomic impact of uveitis on the individual and on the community.
The incidence of uveitis in the United States is approximately 15 cases per 100,000 population per year, or a total of some 38,000 new cases per year. Anterior uveitis is the most common form of uveitis, followed by posterior or panuveitis, intermediate uveitis is the least common form but still comprises a significant number of cases (4% to 17% of all cases of uveitis).
Facts about Uveitis:
- Chronic uveitis is more common than acute and recurrent uveitis.
- Chronic uveitis is especially common in patients with intermediate uveitis.
- Nongranulomatous uveitis occurs more frequently than does granulomatous uveitis, especially in patients with anterior uveitis.
- Noninfectious uveitis is more common than is infectious uveitis, particularly among patients with panuveitis and anterior uveitis.
- Bilateral uveitis (in both eyes) is more common than unilateral uveitis (one eyes) in patients with panuveitis and intermediate uveitis.
- Anterior and posterior uveitis cases have approximately equal distribution of unilateral and bilateral cases.
- The mean age of onset is clearly younger in patients with intermediate uveitis, 30.7 years (+ 15.1 years).
- Despite the huge advances in diagnostic techniques and the determination of ophthalmologists worldwide to reach and etiologic diagnosis, many cases remain in the idiopathic category (35% to 50%). The term idiopathic uveitis denotes that the intraocular inflammation could not be attributed to a specific ocular cause or to an underlying systemic disease, and it was not characteristic of a recognized uveitis entity.
- The most common causes of anterior uveitis are idiopathic (37.8%); seronegative HLA-B27-associated arthropathies (21.6%), juvenile rheumatoid arthritis (10.8%), herpetic uveitis (9.7%) sarcoidosis (5.85%), Fuchs’ heterochromic iridocyclitis (5.0%), systemic lupus erythematosus (3.3%), intraocular lens-induced persistent uvietis (1.2%), Posner-Schlossman syndrome (0.9%), rheumatoid arthritis (0.9%). Syphilis, tuberculosis, phacogenic uveitis, Lyme disease, and collagen vascular disease (Granulomatosis with Polyangiitis (formerly called Wegener’s), polyarteritis nodosa, and relapsing polychondritis) caused some cases of anterior uveitis.
- The most common causes of intermediate uveitis are idiopathic (69.1%), sarcoidosis (22.2%), multiple sclerosis (8.0%), and Lyme disease (0.6%).
- The most common causes of posterior uveitis are toxoplasmosis (24.6%), idiopathic (12.3%), cytomegalovirus retinitis (11.6%), systemic lupus erythematosus (7.9%), birdshot retinochoroidopathy (7.9%), sarcoidosis (7.5%), acute retinal necrosis syndrome (5.5%), Epstein-Barr virus retinochoroiditis (2.9%), toxocariasis (2.5%), Adamantiades-Bechet’s disease (2.0%), syphilis (2.0%), acute posterior multifocal placoid pigment epitheliopathy (2.0%), and serpiginous choroidopathy (1.65%). Other causes of posterior uveitis include punctate inner choroidopathy, multiple evanescent white-dot syndrome, multiple sclerosis, temporal arteritis, presumed ocular histoplasmosis, fungal retinitis, and leukemia.
- The most common causes of panuveitis are idiopathic (22.2%), sarcoidosis (14.1%), multifocal choroiditis and panuveitis (12.1%), ABD (11.6%), systemic lupus erythematosus (9.1%), syphilis (5.5%), Vogt-Koyanagi-Harada syndrome (5.5%), HLA-B72 associated (4.5%), sympathetic ophthalmia (4.0%), tuberculosis (2.0%), fungal retinitis (2.0%). Other causes of panuveitis include bacterial panophthalmitis, intraocular lymphoma, relapsing polychondritis, polyarteritis nodosa, leprosy, dermatomyositis, and progressive systemic scelerosis.
The above-mentioned percentages and figures were obtained from a study of 1237 uveitis patients referred to the Uveitis and Immunology Service of the MEEI, Harvard Medical School, from 1982 to 1992. These figures were found to be similar to the results of other studies of tertiary referral centers from different parts of the world., especially those of developed countries.
See, also, INFLAMMATION, IMMUNE SYSTEM, and AUTOIMMUNE DISEASE, OCULAR IMMUNOLOGIST, CELLS, FLARE, CLASSIFICATION OF UVEITIS, PEDIATRIC UVEITIS, JRA-ASSOCIATED UVEITIS, CELLS, and FLARE
Click and Read
How to Find Medical Information
OTHER LINKS OF INTEREST
- It is likely that both Beethoven and James Joyce had uveitis
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
See, Ocular Immunologist
Inflammation in the blood vessels. It may occur throughout the body.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The ability to distinguish details and shapes of objects; also called central vision.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The entire area that can be seen when the eye is forward, including peripheral vision. The ability to distinguish details and shapes of objects; also called central vision.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Vitritis is the medical term used to denote the accumulation of inflammatory cells or exudates in the vitreous humor, the fluid that fills the middle chamber of the eye, the vitreous chamber. If the pars plana or choroid or optic nerve or retina or retinal vasculature develop inflammation, white blood cells and other by-products of that inflammation, (“inflammatory cells or exudates”), are spilled into the vitreous chamber where the patient can observe “dots” or “floaters“, “streaks” or other “stuff” in their visual field. Thus “vitritis” is actually a symptom of disease occurring in some adjacent structure of the eye. The cells can be counted and form the basis for rating the degree of inflammation in structures in the intermediate part of the eye.
Vitritis is the medical term used to denote the accumulation of inflammatory cells or exudates in the vitreous humor, the fluid that fills the middle chamber of the eye, the vitreous chamber. If the pars plana or choroid or optic nerve or retina or retinal vasculature develop inflammation, white blood cells and other by-products of that inflammation, (“inflammatory cells or exudates”), are spilled into the vitreous chamber where the patient can observe “dots” or “floaters“, “streaks” or other “stuff” in their visual field. Thus “vitritis” is actually a symptom of disease occurring in some adjacent structure of the eye. The cells can be counted and form the basis for rating the degree of inflammation in structures in the intermediate part of the eye.
See, also, CELLS, FLOATERS, INTERMEDIATE UVEITIS, and PARS PLANITIS.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
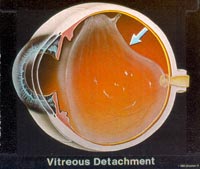 The vitreous is the transparent, colorless, gelatinous mass that fills the space between the lens of the eye and the retina lining the back of the eye. The vitreous is transparent. It contains very few cells, no blood vessels, and 99% of its volume is water. The vitreous is in contact with the retina and helps to keep it in place. The vitreous does not adhere to the retina, except in three places: all around the anterior border of the retina; in the macula, the tiny spot in the retina which gives us our “detail” and central vision; and at the optic nerve disc (where the retina sends one million nerve fibers to the brain).
The vitreous is the transparent, colorless, gelatinous mass that fills the space between the lens of the eye and the retina lining the back of the eye. The vitreous is transparent. It contains very few cells, no blood vessels, and 99% of its volume is water. The vitreous is in contact with the retina and helps to keep it in place. The vitreous does not adhere to the retina, except in three places: all around the anterior border of the retina; in the macula, the tiny spot in the retina which gives us our “detail” and central vision; and at the optic nerve disc (where the retina sends one million nerve fibers to the brain).
Unlike the fluid in the front of the eye (aqueous fluid) which is continuously replenished, the gel in the vitreous chamber is stagnant. Therefore, if cells or other byproducts of inflammation get into the vitreous, they will remain there unless removed surgically (see floaters). If the vitreous pulls away from the retina, it is known as a vitreous detachment. As we age, the vitreous often liquefies and may collapse. This is more likely to occur, and occurs much earlier, in eyes that are nearsighted (myopia). It can also occurs after injuries to the eye or inflammation in the eye (uveitis).
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Vitrectomy is the surgical removal of the vitreous (transparent gel that fills the eye from the iris to the retina). Vitrectomy is a microsurgical procedure in which specialized instruments and techniques are used to repair retinal disorders and to treat intermediate uveitis. This is a major surgical procedure of the eye.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
VOGT-KOYANAGI-HARADA SYNDROME (VKH)
Vogt-Koyanagi-Harada syndrome (VKH), formerly known as uveomenigitic syndrome, is a systemic disorder involving multiple organ systems, including the ocular, auditory, nervous, and integumentary systems. Severe bilateral panuveitis associated with exudative retinal detachment is the hallmark of ocular disease. The disease has worldwide distribution but has predilection for darkly pigmented races such as Asians, Hispanics, and Native Americans. In the United States, 44% in one series were blacks. VKH is uncommon in whites. It is a common cause of endogenous uveitis in Japan, constituting at least 8% of cases. This is also true for certain parts of Latin America, particularly Brazil. In the United States, it accounts for 1% to 4% of all uveitis referrals. Most patients are in the second to fifth decades of life at the onset of the disease. The inflammation is usually granulomatous. Although the exact etiology of VKH is unknown, the disease is thought to be a primarily inflammatory condition directed against melanin-containing cells or a common antigen expressed therein and shared by the skin, eye, meninges, and ear. Alternatively , some investigators have invoked a primary infectious etiology, and others postulate a microbe as initiating or triggering the autoimmune process.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 The fibers (1) that hold the lens (2) suspended in position and enable it to change shape during accommodation. Zonules attach to the ciliary body (3).
The fibers (1) that hold the lens (2) suspended in position and enable it to change shape during accommodation. Zonules attach to the ciliary body (3).