- ACCOMMODATION
- ALGORITHM, TREATMENT ALGORITHM
- AMSLER GRID TEST
- ANGLE CLOSURE GLAUCOMA
- ANKYLOSING SPONDYLITIS (see, HEALTH CONDITIONS)
- ANTERIOR CHAMBER
- ANTERIOR UVEITIS
- ANTIBODY
- ANTIGEN
- APHAKIA
- AQUEOUS HUMOR, AQUEOUS FLUID
- ASTIGMATISM
- AUTOIMMUNE DISEASE
- AUTOIMMUNITY
- CATARACT
- CATARACT AND UVEITIS
- CELLOPHANE MACULOPATHY(EPIRETINAL MEMBRANE)
- CELLS, MEASURE OF UVEITIS ACTIVITY
- CENTRAL RETINAL ARTERY
- CENTRAL RETINAL VEIN
- CENTRAL VISION
- CHEMOTHERAPY
- CHOROID
- CHOROIDITIS
- CHRONIC DISEASE
- CILIARY BODY
- CILIARY MUSCLES
- CILIARY PROCESSES
- CLASSIFICATION OF UVEITIS
- CONES, CONE CELLS
- CONJUNCTIVA
- CONJUNCTIVITIS
- CONTRAST SENSITIVITY
- CORNEA
- CORTICOSTEROIDS
- CYCLITIS
- CYSTOID MACULAR EDEMA (CME)
- ENDOTHELIUM
- EPIRETINAL MEMBRANE (ERM)
- EPISCLERA
- EPISCLERITIS
- EPITHELIUM
- EYE ANATOMY
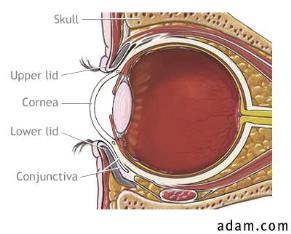
- EYELIDS
A
The ability of the eye to change its focus from distant to near objects; a process achieved by the lens changing its shape.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 The Amsler grid is used by physicians to detect small irregularities in the central 20 degrees of the field of vision. Is a quick and simple test that patients are sometimes asked to use to monitor changes in their vision. For example, It is recommended that people with macular degeneration test their eyes with the Amsler grid several times a week and report changes to their physician.
The Amsler grid is used by physicians to detect small irregularities in the central 20 degrees of the field of vision. Is a quick and simple test that patients are sometimes asked to use to monitor changes in their vision. For example, It is recommended that people with macular degeneration test their eyes with the Amsler grid several times a week and report changes to their physician.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
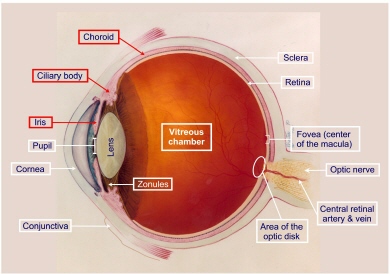
 The anterior chamber of the eye (1) is the space between the cornea (2) and the iris (3). It is filled with fluid called aqueous humor. “Anterior” means “front.”
The anterior chamber of the eye (1) is the space between the cornea (2) and the iris (3). It is filled with fluid called aqueous humor. “Anterior” means “front.”
See, also, POSTERIOR CHAMBER.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Anterior uveitis means inflammation in the anterior (front) geographic area of the eye, bounded by the cornea anteriorly and the iris posteriorly. This inflammation derives primarily from inflammation of the iris. When the iris is inflamed, white blood cells are shed into the anterior chamber. It is these products of inflammation, “cells”, that are observed on slit lamp examination and form the basis for rating the degree of inflammation.
Anterior uveitis means inflammation in the anterior (front) geographic area of the eye, bounded by the cornea anteriorly and the iris posteriorly. This inflammation derives primarily from inflammation of the iris. When the iris is inflamed, white blood cells are shed into the anterior chamber. It is these products of inflammation, “cells”, that are observed on slit lamp examination and form the basis for rating the degree of inflammation.
The International Uveitis Study Group classification schema for uveitis has been widely adopted for clinical and research purposes. It separates uveitis by anatomical location of the disease, according to the major visible signs, in the various segments of the eye: anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis.
See, also, UVEITIS.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Protein that is part of the body’s immune system; it is produced in response to substances, usually foreign, known as antigens. The binding of antibodies to foreign substances facilitates their destruction.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
A substance recognized as foreign by the immune system.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
A person who has no lens inside their eye (whether their own or an artificial one) is aphakic.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
AQUEOUS HUMOR, AQUEOUS FLUID (A-kwe-us)
The aqueous humor is a clear, watery fluid that flows between and nourishes the lens and the cornea. It is secreted by the ciliary epithelium, cells of the ciliary body, and leaves the eye through a passageway known as Schlemm’s Canal.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
ASTIGMATISM (uh-STIG-muh-tizm)
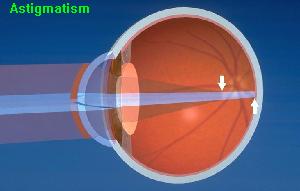 A condition in which the surface of the cornea is not spherical; causes a blurred image to be received at the retina. The irregular shape of the cornea prevents light from focusing properly on the back of your eye, the retina. As a result, your vision may be blurred at all distances.Astigmatism can usually be corrected with glasses or contact lenses.
A condition in which the surface of the cornea is not spherical; causes a blurred image to be received at the retina. The irregular shape of the cornea prevents light from focusing properly on the back of your eye, the retina. As a result, your vision may be blurred at all distances.Astigmatism can usually be corrected with glasses or contact lenses.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
A healthy immune system produces substances called antibodies that help fight and destroy viruses, bacteria, and other foreign substances that invade the body. In autoimmune disorders, the immune system produces antibodies against the body’s healthy cells and tissues. These antibodies, called autoantibodies (“auto” means self), contribute to the inflammation of various parts of the body, including, sometimes, the eye, causing damage and altering the function of target organs and tissues.
In autoimmune diseases, the body harms its own healthy cells and tissues. This leads to inflammation and damage to various body tissues. In addition, some autoantibodies join with substances from the bodyÇs own cells or tissues to form molecules called immune complexes. A buildup of these immune complexes in the body also contributes to inflammation and tissue injury in people with some forms of autoimmune disorder.
Thus autoimmune disease is a disease in which the immune system destroys or attacks the patient’s own body tissue. Regardless of the form of autoimmunity, any autoimmune disease affecting the eye will require systemic (e.g., oral as opposed to local, topical, ocular) therapy; the components of the immune system reside not in the eye, but rather are systemic, and therefore, regulation of those components will require systemic therapy. Such therapy is typically designed to suppress the overly aggressive immune system, allowing the body to eventually re-regulate itself, with the result often being that after the patient has been kept on systemic medications to suppress the inappropriate immune response for a finite length of time (for example, one year), medication can then be tapered and stopped without recurrence of the autoimmune attack. Sometimes resumption of the attack does occur, in which case the patient must be re-treated.
Click and Read
- Multiple Autoimmune Disease
- Ocular Manifestations of Systemic Lupus Erythematosus
- Connection Between Skin Disorders and Ocular Disease
- Association of Ocular Inflammatory Disease with Inflammatory Bowel Disease
- Ocular Sarcoidosis
- It appears likely that Beethoven had sarcoid-related uveitis
- Understanding the Immune System (NIH)
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Under normal conditions, the immune system protects the body from diseases and infections by killing harmful “foreign” substances, such as germs, that enter the body. Autoimmunity is a condition in which the immune system mistakenly attacks and harms the body’s own cells and tissues; this immune reaction is the basis of a variety of autoimmune diseases including some forms of uveitis, diabetes, rheumatoid arthritis, and systemic lupus erythematosus, among others. Uveitis on the basis of autoimmunity is the most common form of uveitis.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Deposition of calcium in the cornea associated with degenerative corneal disease, high blood calcium levels and juvenile arthritis and chronic uveitis.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
BIRDSHOT RETINOCHOROIDOPATHY (BSRC)
Birdshot retinochoroidopathy is a chronic intraocular inflammatory disease affecting mainly the posterior segment of the eye. It is distinct from other forms of posterior uveitis because of a very characteristic clinical presentation and a strong association with HLA-A29.2 antigen. Its etiology remains unknown. An autoimmune mechanism is likely to play an important pathogenic role given the demonstration of retinal autoantigen reactivity and the very strong association with the human leukocyte antigen (HLA)-A29 phenotype unique to this disease.
BSRC is an uncommon disease. In contrast to most other uveitic entities in which the onset of disease is in younger age groups, BSRC typically occurs during middle age, presenting at an average age of 50, with a range of between 35 and 70 years of age. The reason for this age shift is unclear. BSRC is found almost exclusively among whites, with a higher incidence in those of Northern European descent. An apparent gender preference is observed in some series, with women representing up to 70% of reported cases, whereas no significant predilection for sex is found in other series.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Each eye looking at the same object sees a slightly different image. Binocular vision is the ability to fuse these two images into one and gives us the ability to perceive depth and judge distances.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
BLEPHARITIS (INFLAMMATION OF THE EYELIDS)
 Blepharitis refers to an inflammation in the oily glands of the eyelid. This usually results in swollen eyelids and excessive crusting of the eyelashes, most evident in the morning. Tenderness of the eyelids and a foreign body sensation in the eye may occur as well. Blepharitis is a chronic or long term inflammation of the eyelids and eyelashes. It affects people of all ages. Among the most common causes of blepharitis are poor eyelid hygiene; excessive oil produced by the glands in the eyelid; a bacterial infection (often staphylococcal); or an allergic reaction.
Blepharitis refers to an inflammation in the oily glands of the eyelid. This usually results in swollen eyelids and excessive crusting of the eyelashes, most evident in the morning. Tenderness of the eyelids and a foreign body sensation in the eye may occur as well. Blepharitis is a chronic or long term inflammation of the eyelids and eyelashes. It affects people of all ages. Among the most common causes of blepharitis are poor eyelid hygiene; excessive oil produced by the glands in the eyelid; a bacterial infection (often staphylococcal); or an allergic reaction.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
1) A small area of the visual field where the optic nerve enters the eye; occurs normally in all eyes. 2) Any gap in the visual field corresponding to an area of the retina where no visual cells are present; associated with eye disease.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Bruch’s membrane, shown here in yellow, separates the blood vessels of the choroid (on right) from the RPE layer (on left) of the retina. Picture from New York Eye and Ear.
Bruch’s membrane, shown here in yellow, separates the blood vessels of the choroid (on right) from the RPE layer (on left) of the retina. Picture from New York Eye and Ear.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Inside the eye, there is a lens which helps us to focus on what we see. The lens is made mostly of water and protein. The protein is arranged to let light pass through and focus on the retina.
Sometimes some of the protein clumps together and starts to cloud a small area of the lens.This cloudiness of the lens is called a cataract. Over time, the cataract may grow larger and cloud more of the lens as shown in the photograph below, making it more difficult to see. In the early stages, stronger lighting may lessen the vision problems caused by cataracts. At a certain point, however, surgery may be needed to improve vision.
 Today, cataract surgery is safe and very effective. Although researchers are learning more about cataracts, no one knows for sure what causes them. The most common type of cataract is related to aging. More than half of all Americans age 65 and older have a cataract. Scientists think there may be several causes, including smoking and diabetes. Or, it may be that the protein in the lens just changes as it ages. There is also some evidence that cataracts are linked to certain vitamins and minerals. The National Eye Institute (NEI) is doing a study to see whether taking more of these substances prevents or delays cataracts.
Today, cataract surgery is safe and very effective. Although researchers are learning more about cataracts, no one knows for sure what causes them. The most common type of cataract is related to aging. More than half of all Americans age 65 and older have a cataract. Scientists think there may be several causes, including smoking and diabetes. Or, it may be that the protein in the lens just changes as it ages. There is also some evidence that cataracts are linked to certain vitamins and minerals. The National Eye Institute (NEI) is doing a study to see whether taking more of these substances prevents or delays cataracts.
Cataract develops in patients with uveitis because of the uveitis itself and also because of the prolonged use of steroid medications. Cataract developing in an eye with a history of chronic or recurrent uveitis has historically been called cataracta complicata.
 The picture on the right is of a subcapsular cataract. A subcapsular cataract is often found in people taking steroids. Subcapsular cataract develops slowly and starts as a small opacity, usually at the back of the lens. Significant visual symptoms may not appear until the cataract is well developed. Typical symptoms are glare and blur.
The picture on the right is of a subcapsular cataract. A subcapsular cataract is often found in people taking steroids. Subcapsular cataract develops slowly and starts as a small opacity, usually at the back of the lens. Significant visual symptoms may not appear until the cataract is well developed. Typical symptoms are glare and blur.
Photos courtesy of The Lighthouse Inc., (Lighthouse National Center for Vision and Aging) New York, NY
Click and Read
- Cataract
- Cataract Surgery and Uveitis
- Cataract Development and Cataract Surgery in Patients with Juvenile Rheumatoid Arthritis-associated Iridocyclitis. Foster CS, Barrett F. 1993. . Ophthalmology, 100:809-817.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
See, EPIRETINAL MEMBRANE
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
CELLS, A MEASURE OF UVEITIS ACTIVITY
| Ophthalmologists use the term “cells” to refer to white blood cells (leukocytes) that can be observed during the slit lamp examination of the front of the eye (the anterior chamber). Cells are a byproduct of inflammation. If structures in the front of the eye have inflammation, cells are shed into the fluids in the front chamber of the eye (into the aqueous humor), and can be observed and counted in the narrow beam of light from the slit lamp. This cell count forms the basis for grading the severity of inflammationat any given point in time.The number of white blood cells is used as a measure of uveitis activity, and is scaled from 1 to 4, depending on the severity (1 being the least severe inflammation and 4 being the most severe inflammation). The right hand table is the grading of aqueous cells in anterior uveitis used by most uveitis specialists. |
|
|||||||||||||||||||||
Inflammatory cells in the anterior chamber are usually a result of inflammation of the iris. Cells are difficult to capture in photographs and, thus, we do not have a picture to show you. If you have ever noticed dust in the air as light passes through a shutter, you have a bit of an idea of what “cell” look like floating in the front of the eye.
See, also, FLARE.
Cells can also be observed in the vitreous (the middle chamber of the eye) on dilated examination. Inflammatory cell accumulation in the vitreous is the result of inflammatory process in other parts of the eye such as the ciliary body, retina, and choroid.
Cells in the vitreous can be living or dead, and both can become immutably affixed to vitreous fibers. Only live, active cells are graded in the MERSI rating system. Vitreous cells are rated on a scale of 1-4 , as follows: 1/2+=1-10 cells. 1+=11-20 cells. 2+=20-30 cells. 3+=30-100 cells. 4+=grater than 100 cells. Other institutions use other rating systems to grade vitreous cells.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The blood vessel that carries blood into the eye; supplies nutrition to the retina.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The blood vessel that carries blood from the retina.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
See visual acuity.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
See IMMUNOSUPPRESSIVE CHEMOTHERAPY
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
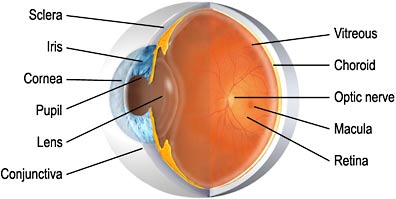
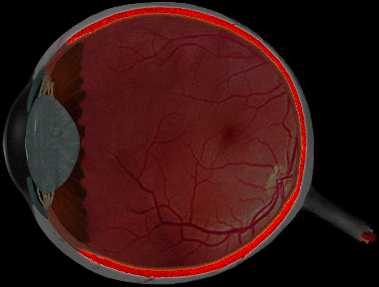 The choroid, shown here in bright red, lies between the retina and sclera. The choroid is a soft, thin, brown, extremely vascular layer, lining the inner surface of the sclera. It is composed of layers of blood vessels that nourish the back of the eye. The choroid connects with the ciliary body toward the front of the eye and is attached to edges of the optic nerve at the back of the eye. The principal function of the choroid lies in the blood nourishment of the outer layers of the retina. The choroid is part of the uvea. Inflammation in this layer of the eye is called choroiditis.
The choroid, shown here in bright red, lies between the retina and sclera. The choroid is a soft, thin, brown, extremely vascular layer, lining the inner surface of the sclera. It is composed of layers of blood vessels that nourish the back of the eye. The choroid connects with the ciliary body toward the front of the eye and is attached to edges of the optic nerve at the back of the eye. The principal function of the choroid lies in the blood nourishment of the outer layers of the retina. The choroid is part of the uvea. Inflammation in this layer of the eye is called choroiditis.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Inflammation of the choroid, the middle layer of the eye composed of blood vessels that nourish the back of the eye.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
CHRONIC DISEASE, CHRONIC ILLNESS
An illness that lasts for a long time. With regard to uveitis, inflammation lasting greater than 3 months or which recurs intermittently. Chronic means that the inflammation is there all the time, every day, day in and day out, to one degree or other. Recurrent means that the inflammation may be gone for a while and then recur.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 The ciliary body the structure behind the iris responsible for making aqueous humor, the fluid in the eye that nourishes the lens and cornea. The ciliary body is divisible into two parts: the pars plana and the pars plicata anteriorly.
The ciliary body the structure behind the iris responsible for making aqueous humor, the fluid in the eye that nourishes the lens and cornea. The ciliary body is divisible into two parts: the pars plana and the pars plicata anteriorly.
The ciliary body is part of the uveal tract. In the diagram below, the uveal tract is shown in red (Iris, ciliary body, and choroid). The ciliary body is nourished by blood vessels which also supply the iris.
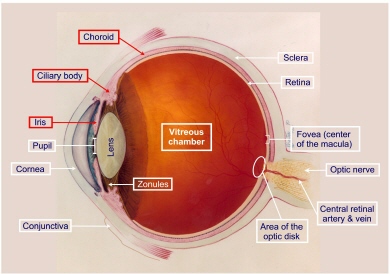 The ciliary body attaches to the iris at the iris root, and, at the ora serrata, posteriorly, the ciliary body joins the posterior continuation of the uvea, the choroid.
The ciliary body attaches to the iris at the iris root, and, at the ora serrata, posteriorly, the ciliary body joins the posterior continuation of the uvea, the choroid.
The ciliary body supports the lens through the zonules.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The ciliary muscles relax the zonules to enable the lens to change shape (become more spherical) for focusing at near. The ciliary muscles make the lens thicker so the eye can focus on nearby objects and thinner so the eye can focus on distant objects.
See, also, CILIARY BODY.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The extensions or projections of the ciliary body that secrete aqueous humor.
See, also, CILIARY BODY.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
WHY ARE THERE SO MANY DIFFERENT NAMES FOR UVEITIS?
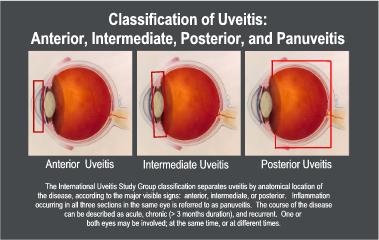
Uveitis is inflammation inside the eye, specifically affecting one or more of the three parts of the eye that make up the uvea: the iris (the colored part of the eye), the ciliary body (behind the iris, responsible for manufacturing the fluid inside the eye) and the choroid (the vascular lining tissue underneath the retina).
These structures, shown in the diagram in pink, are collectively known as the uveal tract. There are many different names for uveitis. Readers to this site, for example, may have been told that they have a condition known as iritis, or iridocyclitis, or uveitis, or plars planitis, or choroiditis, or retinitis, to name a few.The International Uveitis Study Group recommended a classification schema that has been widely adopted for clinical and research purposes. It separates uveitis by anatomical location of the disease, according to the major visible signs, in the various segments of the eye: anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis. The course of the disease can be be further described as acute, chronic (> 3 months duration), and recurrent.
Classification of uveitis is important for the following reasons:
- The uvea consists of three continuous but distinct parts. One or more parts of the uvea may be inflamed, but others may not. In some cases, all three parts of the uvea are affected.
- Uveitis may be caused by a vast number of highly variable conditions. Treatment and prognosis of one entity may be completely different from that of another (e.g. infectious uveitis and autoimmune uveitis).
- Uveitis nay be one of the features of a serious or life-threatening systemic disease (e.g., systemic vasculitis). In some cases, uveitis is the presenting feature of such a disease. Proper diagnosis and treatment of the uveitis and of the systemic condition can enormously enhance quality of life and reduce mortality.
- Uveitis is an entity for which no causative agent may be found, despite the most thorough diagnostic investigations, in a number of cases. Accurately describing, characterizing, and classifying such cases may eventually help researchers and clinicians in elucidating the nature of such diseases.
- Proper classification is essential if one is to avoid confusion and misinterpretation. The anatomic classification should not be confused or overlap with the etiologic classification. Both classifications are required and important, but they are distinct and different.
WHAT IS THE DIFFERENCE BETWEEN “UVEITIS” AND “OCULAR INFLAMMATORY DISEASE”?
Uveitis is one type, or sub-group, of ocular inflammatory disease. The uveal tract is not the only place in the eye where Inflammation occurs. Inflammation can occur inside the eye itself, or in the tissue, nerves, muscles or structures that surround the eye. This comprises a large group of diverse diseases collectively known as ocular inflammatory disease (OID). Ocular immunologists specialize in treating all forms of ocular inflammatory disease.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Cones are one type of specialized light-sensitive cells (photoreceptors) in the retina that provide sharp central vision and color vision. Also see rods. The retina contains approximately 6 million cones. The cones are contained in the macula, the portion of the retina responsible for central vision. They are most densely packed within the fovea, the very center portion of the macula. Cones function best in bright light and allow us to appreciate color.
Cones are one type of specialized light-sensitive cells (photoreceptors) in the retina that provide sharp central vision and color vision. Also see rods. The retina contains approximately 6 million cones. The cones are contained in the macula, the portion of the retina responsible for central vision. They are most densely packed within the fovea, the very center portion of the macula. Cones function best in bright light and allow us to appreciate color.
Cones are one type of specialized light-sensitive cells (photoreceptors) in the retina that provide sharp central vision and color vision. Also see rods. The retina contains approximately 6 million cones. The cones are contained in the macula, the portion of the retina responsible for central vision. They are most densely packed within the fovea, the very center portion of the macula. Cones function best in bright light and allow us to appreciate color.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
CONJUNCTIVA (KAHN-junk-TY-vuh)
 The conjunctiva is the thin, transparent tissue that covers the outer surface of the eye. It begins at the outer edge of the cornea, covering the visible part of the sclera, and lining the inside of the eyelids. It is nourished by tiny blood vessels that are nearly invisible to the naked eye. The conjunctiva also secretes oils and mucus that moisten and lubricate the eye.
The conjunctiva is the thin, transparent tissue that covers the outer surface of the eye. It begins at the outer edge of the cornea, covering the visible part of the sclera, and lining the inside of the eyelids. It is nourished by tiny blood vessels that are nearly invisible to the naked eye. The conjunctiva also secretes oils and mucus that moisten and lubricate the eye.
Click and Read
- Ocular Cicatricial Pemphigoid
- Cataract Surgery in Ocular Cicatricial Pemphigoid
- Episodic Conjunctival Inflammation after Stevens-Johnson Syndrome
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent layer that lines the inner eyelid and covers the white part of the eye, the sclera.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The ability to perceive differences between an object and its background.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
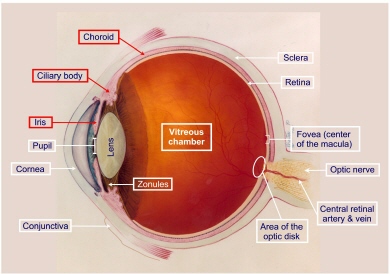
The cornea is the outer, transparent, dome-like structure that forms the anterior most part of the outer coat of the eye. Looking through the cornea, as through a window, one can see the iris, pupil, and anterior chamber. The cornea is part of eye’s focusing system.
Click and Read
- Keratitis: Corneal Inflammation
- Growth Factors and Corneal Wound Healing
- Corneal Transplantation and Immunologic Tolerance
- Reports: Rosacea and PUK
- Reports: Mooren’s Ulcer: Diagnosis and Management
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
CORTICOSTEROIDS (STEROID MEDICATIONS)
Corticosteroids (kor-ti-koe-STER-oyds) (cortisone-like medicines) are prescribed medications used to provide relief for inflamed areas of the body, including the eyes. They lessen swelling, redness, itching, and allergic reactions. Corticosteroids are often used as part of the treatment for a number of different diseases, such as severe allergies or skin problems, asthma, arthritis, and eye inflammation. Your body naturally produces certain cortisone-like hormones that are necessary to maintain good health. Patients who do not produce enough of these hormones may have had the medication prescribed to help make up the difference.
Corticosteroids are very strong medicines. In addition to their helpful effects in treating medical problems, they have side effects that can be very serious. Long-term use of steroid medications in the treatment of ocular inflammatory disease is associated with the formation of cataract, and, in some individuals, a rise in intraocular pressure that can lead to glaucoma, with irreversible damage to the optic nerve and loss of vision.
Steroid use in eye care includes administration in eye drops, by injection and infusion, or as an oral medication taken daily. Because of the undesirable side effects of long-term use of steroid, patients with ocular inflammatory disease are advised to discuss the use of steroid-sparing treatments with their treating ophthalmologist BEFORE permanent structural damage to the eye occurs.
| Common Steroid Medications in USA (Eye Drops) | ||
|
|
||
| Product Name | Generic Name | Manufacturer |
|
|
||
| Pred Forte 1% | Prednisolone acetate | Allergan |
| Pred Mild 0.12% | Prednisolone acetate | Allergan |
| Vexol 1% | Rimexolone | Alcon |
| Flarex 0.1% | Fluorometholone acetate | Alcon |
| Eflone 0.1% | Fluorometholone acetate | Ciba Vision |
| FML SOP (ointment) | Fluorometholone alcohol | Allergan |
| Fluor-Op 0.1% | Fluorometholone alcohol | Ciba Vision |
| FML Liquifilm 0.1% | Fluorometholone alcohol | Allergan |
| Decadron 0.05% | Dexamethasone sodium phosphate | Merck |
| Maxidex 0.05% | Dexamethasone sodium phosphate | Alcon |
| Ocu-Dex 0.05% | Dexamethasone sodium phosphate | Ocumed |
| Lotemax 0.5% | Loteprednol etabonate | Bausch & Lomb |
|
|
||
See, also, GLAUCOMA and CATARACT.
Click and Read:
- Treatment guidelines (algorithms) for ocular inflammatory disease
- Immunomodulatory Therapy for Children with Steroid-Resistant
and Steroid-Dependent Uveitis - Intraocular Pressure in Steroid Injections
- Prescription Drug Patient Assistance Programs in the United States
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Cyclitis is inflammation of the ciliary body, the structure responsible for production of aqueous humor and for changes in the shape of the lens. See, also, IRIDOCYCLITIS.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
See MACULAR EDEMA.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
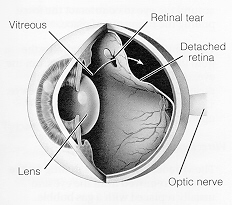 A retinal detachment occurs when the retina is pulled away from its normal position in the back of the eye. The retina sends visual images to the brain through the optic nerve. When detachment occurs, vision is blurred. A detached retina is a very serious problem that almost always causes blindness unless it is treated.Detachments can be from tears or holes in the retina, or from fluid accumulation between the retina and underlying layers. When there is a tear of the retina, liquid from the vitreous may pass through the tear, and detach the retina. As the fluid accumulates, the retinal detachment becomes larger. Detached areas of the retina lose their vision. Most people notice floaters and flashes before the retina detaches. As the detachment occurs, a gradually enlarging dark area may be seen. Anyone with flashes or the sudden onset of a new floater (or floaters) should be examined promptly by an ophthalmologist. The ophthalmologist will search carefully for retinal tears.
A retinal detachment occurs when the retina is pulled away from its normal position in the back of the eye. The retina sends visual images to the brain through the optic nerve. When detachment occurs, vision is blurred. A detached retina is a very serious problem that almost always causes blindness unless it is treated.Detachments can be from tears or holes in the retina, or from fluid accumulation between the retina and underlying layers. When there is a tear of the retina, liquid from the vitreous may pass through the tear, and detach the retina. As the fluid accumulates, the retinal detachment becomes larger. Detached areas of the retina lose their vision. Most people notice floaters and flashes before the retina detaches. As the detachment occurs, a gradually enlarging dark area may be seen. Anyone with flashes or the sudden onset of a new floater (or floaters) should be examined promptly by an ophthalmologist. The ophthalmologist will search carefully for retinal tears.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
A process by which the pupil is temporarily enlarged with special eye drops (mydriatic); allows the eye care specialist to better view the inside of the eye.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Tiny yellow or white deposits in the retina or optic nerve head.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
DRY EYE (KERATOCONJUNCTIVITIS SICCA)
Dry eye is a condition that can develop under many circumstances. Dry eye affects an estimated 10 million people or more in the United States alone. In some, it may be associated with underlying medical problems. The dry eye syndrome is caused by the alteration in one’s natural tear film, a thin layer of tears protecting the surface of our eyes. Damage to the surface of the eyes (cornea and conjunctiva) is responsible for the symptoms of dry eyes.
Aside from the wearing of contact lenses, perhaps the most important cause of dry eye is the natural aging process. At age 65, the eye produces about 60% fewer tears than it did at age 18. But dry eye can also result from disruption of the blinking reflex, medications such as antihistamines, decongestants, and heart medications, vitamin A deficiency, and environmental factors (sun, wind, smoke, and air conditioners). Even low humidity or high atmospheric pressures can produce dry eye in some individuals. Autoimmune disease can also cause “dry eye” (see SJOGREN’S SYNDROME).
Click and Read
- Dry Eye
- Epstein Barr Virus Dacryoadenitis Resulting in Keratoconjunctivitis Sicca in a Child
- NIH Information Sheet: What is Sjogren’s Syndrome
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The inner layer of cells on the inside surface of the cornea.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
EPIRETINAL MEMBRANE (ERM) (MACULAR PUCKER)
An epiretinal membrane is, generally, a thin layer of collagen on the surface of the retina. It may occur spontaneously.
It may occur after vitrectomy for detached retina. It may occur because of inflammation (uveitis). It usually occurs on or near the macula, and therefore affects vision.If it is extremely thin, some call it a “cellophane maculopathy” when it is on the macula. If it contracts (and collagen or scar tissue often does), it distorts the photoreceptors or light-sensing neural elements of the macula, producing “macular pucker”. But even without contraction and pucker an ERM can and usually does affect vision. They almost never, ever disappear spontaneously. They can be removed surgically, ERM “peeling”. This procedure is “high risk”, i.e. one can end up worse off rather than improved after such surgery; imagine peeling Scotch tape (the ERM) off tissue paper (the macula). And, so most retinal surgeons who perform ERM peeling rarely attempt such an operation unless the patient’s vision is pretty poor, say 20/80 or worse; each surgeon typically has his or her own criterion or “cut-off” level of vision below which the risk of surgery is deemed too great for the potential benefit to be gained.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The outermost layer of cells of the cornea and the eye’s first defense against infection.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
A thin layer of tissue containing many blood vessels that nourish the sclera. At the front of the eye, the episclera is covered by the conjunctiva.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Inflammation of the episclera, a membrane covering the sclera of the eye. The episclera is a thin layer of tissue containing many blood vessels that nourish the sclera. At the front of the eye, the episclera is covered by the conjunctiva. Episcleritis is a non-infectious inflammation of the episclera. Episcleritis is usually mild and rarely progresses to scleritis.
Click and Read
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
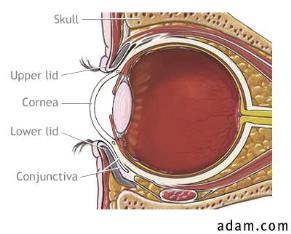 The eyelids play a key role in protecting the eyes. They help spread moisture (tears) over the surface of the eyes when they close (for example, while blinking); thus, they help prevent the eyes from becoming dry. They also maintain a smooth corneal surface by spreading tears evenly over the eye. The lids are composed of an outer layer of skin, a middle layer of muscle and tissue that gives them form, and an inner layer of moist conjunctival tissue.
The eyelids play a key role in protecting the eyes. They help spread moisture (tears) over the surface of the eyes when they close (for example, while blinking); thus, they help prevent the eyes from becoming dry. They also maintain a smooth corneal surface by spreading tears evenly over the eye. The lids are composed of an outer layer of skin, a middle layer of muscle and tissue that gives them form, and an inner layer of moist conjunctival tissue.
The eyelids also provide a mechanical barrier against injury, closing reflexively when an object comes too close to the eye. The reflex is triggered by the sight of an approaching object, the touch of an object on the surface of the eye, or the eyelashes being exposed to wind or small particles such as dust or sand.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Flare is protein in the anterior chamber from leakage from inflamed blood vessels in the iris. It is not always a measure of uveitis activity. Flare is measured on a scale from 1 to 4, with 4 being the most severe. Flare gives the aqueous a particulate, or smoky, appearance as can be observed in the photograph. Flare becomes chronic after uveitis has produced permanent changes to blood vessels, and so “flare” may be present even when the patient is not having a “flare-up” of his or her uveitis.
Flare is protein in the anterior chamber from leakage from inflamed blood vessels in the iris. It is not always a measure of uveitis activity. Flare is measured on a scale from 1 to 4, with 4 being the most severe. Flare gives the aqueous a particulate, or smoky, appearance as can be observed in the photograph. Flare becomes chronic after uveitis has produced permanent changes to blood vessels, and so “flare” may be present even when the patient is not having a “flare-up” of his or her uveitis.
Flare in the vitreous can also be observed and rated.
See, also, CELLS.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
Flashes are sensations of light, when no light is really there. They may appear as many tiny bright lights (like “sparklers”) or like flashes of lightening. Flashes may occur when the vitreous jelly pulls on or tears the retina. These flashes usually last for only a second or so, but typically occur repeatedly. They may be more obvious with eye movement, or in a dark room. Anyone with flashers should be examined promptly by an ophthalmologist. The ophthalmologist will search carefully for retinal tears.
Some people with migraine headaches may experience a different type of flash. These are usually shimmering, jagged lights that are present constantly for a period of fifteen minutes or so. They typically appear in the center of your field of vision, and progress slowly towards the edges of the visual field. A headache that is commonly throbbing, and on one side of the head, may follow the disappearance of the flashes.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
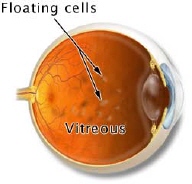 Floaters appear as gray or black specks, strands, or “cobwebs” in front of the eyes. As the eyes move, the floaters move too. They do not follow your eye movements precisely, as they usually drift when the eyes start or stop moving. Floaters are caused by particles, such as white blood cells and vitreous condensates, suspended in the vitreous gel, the clear, jelly-like fluid that fills the inside of the eye.The floaters cast shadows on the light sensitive retina. It is actually the shadow of the floater that you see. Floaters may have a variety of causes, some serious, and some not serious at all. New floaters can be an indication of recurrence of uveitis and patients should see their physician for an examination if sudden changes in the appearance or number of floaters is noticed.
Floaters appear as gray or black specks, strands, or “cobwebs” in front of the eyes. As the eyes move, the floaters move too. They do not follow your eye movements precisely, as they usually drift when the eyes start or stop moving. Floaters are caused by particles, such as white blood cells and vitreous condensates, suspended in the vitreous gel, the clear, jelly-like fluid that fills the inside of the eye.The floaters cast shadows on the light sensitive retina. It is actually the shadow of the floater that you see. Floaters may have a variety of causes, some serious, and some not serious at all. New floaters can be an indication of recurrence of uveitis and patients should see their physician for an examination if sudden changes in the appearance or number of floaters is noticed.
See, also, VITRITIS.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 Flourescein angiography (FLOR-uh-seen an-jee-AHG-ruh-fee) is a test to examine blood vessels in the retina, choroid, and iris. A special dye is injected into a vein in the arm and pictures are taken as the dye passes through blood vessels in the eye.
Flourescein angiography (FLOR-uh-seen an-jee-AHG-ruh-fee) is a test to examine blood vessels in the retina, choroid, and iris. A special dye is injected into a vein in the arm and pictures are taken as the dye passes through blood vessels in the eye.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
The central part of the macula that provides the sharpest vision.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]
 The posterior part, or back, of the eyeball, which includes part of the retina, optic disc, and macula; portion of the inner eye that can be seen during an eye examination by looking through the pupil with the ophthalmoscope. The photograph is of a normal fundus.
The posterior part, or back, of the eyeball, which includes part of the retina, optic disc, and macula; portion of the inner eye that can be seen during an eye examination by looking through the pupil with the ophthalmoscope. The photograph is of a normal fundus.
A–B–C–D–E–F–G–H–I–J–K–L–M–N–O–P–Q–R–S–T–U–V–W–X–Y–Z [Browse Terms] [Top]